Editor’s note: This text-based course is an edited transcript of the webinar, IEP and IFSP 101: Everything You Need to Know - Planning to Implementation, presented by Laura Ritter, MA.
Learning Outcomes
After this course, participants will be able to:
- List at least five IDEA categories to qualify for special services.
- Define at least three key terms commonly used during IFSP/IEP meetings.
- Identify at least four IFSP/IEP legal requirements.
Introduction
We often use many terms in the school setting, such as IEPs, 504 plans, accommodations, and modifications, but I've found that many teachers are unfamiliar with what these terms really mean. I've had a lot of teachers frequently asking questions such as:
- How is the IEP written?
- What is needed for the IEP meeting?
- How do you follow through with a plan, once it's put into place?
My hope today is that the information shared will clear up some of those questions and help you feel more comfortable with the IFSP and IEP planning and implementation process.
IEP/IFSP - What Does That Mean?
So what does all this mean? An IEP is an Individualized Education Program, although it's sometimes referred to as an Individualized Education Plan. An IFSP is an Individualized Family Service Plan which serves younger children from infancy through two years old.
Individualized Family Service Plan (IFSP)
First, we will cover the Individualized Family Service Plan. The IFSP should guide and support the entire family as the parents are a vital part of this process. Again, these are serving the younger children so, at this age, the parents really need to be involved and they're wanting to find the best situation for their child.
The IFSP team typically involves the parents, service coordinator, and various specialists, such as occupational therapists, speech-language pathologists, or physical therapists. This might even include your family physician. There is a wide range of services that are available for a child qualifying for an IFSP such as speech services, nutrition services, and developmental therapy. Personally, I found this really helpful for my youngest son who needed speech services. The coordinator set up meetings and they came to my house for those meetings. It was a much more intimate situation than we'll talk about later on once the child is in the school.
The IFSP team will review the plan bi-annually and make revisions annually. Once a year the team will get together to come up with new goals for the coming year, but it is important to review those goals bi-annually. In addition to that, progress updates should be provided to the family quarterly. When my son had an IFSP it was really helpful, even though I'm an educator, that the therapist talked with me and told me quarterly how my son was doing and what she was working on.
It is important to note that parents are legally entitled to change or even decline services throughout the IFSP process. This is different from the IEP that we'll talk about later on, which is a legally binding document. At the IFSP level, since the children are so young and the parents are involved, they can make changes at any point in time. Even though the goals might be set for a year, it is okay if the parents change their minds and say they'd actually like to see their son or daughter doing this and maybe we could work on this. Again, this is a team decision, but the parents are an intricate part of this process.
What happens next?
After the child has been receiving services, he or she will be re-evaluated before the child turns three to determine if services are still needed into school age. This can be confusing because you sometimes hear that the IFSP goes until a child is two years old. The plan is in effect until the day before the child's third birthday. If the team decides that services are still needed for the child, the special education teacher and specialists will meet with the family to develop an IEP for the school system. The IEP will take effect on the day the child turns three.
For example, if the child had speech services and the family and team still felt like the child needed more services after the child turned three, then the team would come together with someone from the school system and meet again to continue services at the school. Typically, the IFSP services are provided in the home, but once the child turns three services are often provided at the school.
Qualifying Disability Categories
- Autism Spectrum Disorder (ASD)
- Intellectual Disability (ID)
- Deaf-Blindness
- Deafness
- Emotional Disturbance (ED)
- Hearing Impairment (HI)
- Multiple Disabilities
- Orthopedic Impairment (OI)
- Other Health Impairment (OHI)
- Specific Learning Disability (SLD)
- Speech or Language Impairment
- Traumatic Brain Injury (TBI)
- Visual Impairment (VI)
- Includes Blindness
The legal guidelines that the school system follows are classified under the Individuals with Disabilities Education Act (IDEA). There are 13 qualifying disability categories to identify for special education services and to receive an IEP. Now we're talking about a child who is three years old or older. The team has decided that the child's going to need continued services or this might be referring to a child that hasn't had services before. If it's a child who hasn't had services yet there would be an initial evaluation and the team would try to determine whether the student meets one of these 13 IDEA categories. We're going to go over these 13 categories and I encourage you to read more about them because I will just be scratching the surface today. Under the Individuals with Disabilities Education Act (IDEA), every child has a legal right to a free and appropriate public education (FAPE). Let's break down each of these 13 categories.
Autism Spectrum Disorder (ASD)
The first category is autism spectrum disorder. Students with autism typically exhibit a wide range or spectrum of characteristics and symptoms. The word spectrum comes from the fact that there are so many different characteristics that you'll see in a child with autism. It can range from mild to severe. Typically, students with autism express difficulty with social skills and communication. Students might even be nonverbal. Teachers might be working with students using visuals or tangible items to help them express their wants and needs.
For example, I had a student that really loved Paw Patrol and that was the only thing he wanted. All he wanted to do throughout the day was to watch the show Paw Patrol, so I used that as a reinforcer and as a way to get him to communicate. If he was asking for it, I would want him to do more than just point to the TV. I really wanted to bring that communication out, so I had a Paw Patrol DVD in the room. I would give two choices: the Paw Patrol DVD or a sock. It could be anything. At first, when you're trying to work on communication, having two extreme opposites is a great tool, because they say clearly, "I want the Paw Patrol DVD, not the sock." The hope is that they bring you the DVD. This is just one tip for trying to promote communication in the classroom. That's an example of someone that might be a bit more severe and needs help with communication skills.
You will often see students with autism who engage in excessive, repetitive behaviors. This could be any behavior from clapping their hands a hundred times a day or jumping up and down over and over. It could be the same motion that happens over and over, such as hand flapping or watching their fingers move. Typically, teachers try to work with the student and the families on how to replace that behavior, especially if it is a negative type of behavior such as pinching or scratching. One replacement behavior is to hold a fidget item in their hand instead of using their hands in a negative way.
Typically, children with autism are diagnosed at a young age. This is different than some other disabilities that we'll talk about. Doctors are really working with families at a young age to see if they're having any of the symptoms of autism spectrum disorder. This is true even for children under three years old in the IFSP levels that we were discussing. Doctors want to see the benchmarks even before they get to be school-aged.
Intellectual Disability (ID)
Another category under the IDEA is the intellectual disability category. Up until 2010, this category was referred to as mental retardation (MR). This was a big change in the IDEA laws and in the medical journals. Now when you look up something that's older you might still see it referred to as MR but they've tried to change everything to use the term intellectual disability instead of mental retardation. Students identified in this category typically have limited intellectual and adaptive functioning. Students with intellectual disabilities are not typically completing the same coursework as their same-age peers.
There are four degrees of this disability category: mild, moderate, severe, and profound. Students that fall in the severe and profound levels will have much more limited intellectual and adaptive functioning. Their IQ is typically below 70 and they need much more support than people in some of the other IDEA categories that we'll discuss.
An example of an intellectual disability might be a student with Down syndrome. As we will discuss later, the least restrictive environment is important for these students because we really want to find out how long they can be in the regular classroom. Do they need time away from the classroom, such as in a separate resource room or a life skills type of classroom? The goal is to have inclusion as much as possible for these students and for students in all of the disability categories that we're discussing.
Deaf-Blindness
The next category for the IDEA is deaf-blindness. Students have a combination of sight and hearing loss in deaf-blindness, so this is the student that has some vision and audible range, but in order to be classified under this category they must exhibit some deafness and blindness. Students will need additional support outside their classroom programs such as educational audiologists, speech pathologists, and vision specialists. You might be thinking, "What if we don't have these types of specialists in our school?"
That's why, as we talk about the IEP and the legally binding document that it is, when something's written in the plan, it is the responsibility of the school system, the school, and anyone involved to get the child the services that he or she needs. If your student needs a vision specialist and you don't have one in the school, then it is up to the administrators in the special education department to find the specialists and the services that the student needs.
Deafness
Students identified in the category of deafness will have hearing loss in the severe to profound levels. Typically, hearing loss above 90 decibels is considered deafness. It does not necessarily impede the child's cognitive ability. Students can perform at the same level academically as their same-age peers, but they will need more assistance in the classroom. Again, with the least restrictive environment, the goal is that the child will be able to perform in the classroom with his or her peers, but might need assistive technology or hearing devices. These supports can significantly improve the classroom experience. Teachers could provide additional resources to the students, such as more PowerPoint presentations or printed handouts instead of everything having to be heard through the speech of the teacher. Visuals are great for these students.
Emotional Disturbance (ED)
The disability category of emotional disturbance can be difficult to diagnose at times because it can be a bit more objective than diagnosing hearing or vision loss. Diagnosing emotional disturbance takes the team, including medical professionals, to work with the family on the emotional disturbance disability classification.
According to the Individuals With Disabilities Education Act (IDEA), an emotional disturbance is defined as "a condition exhibiting one or more of the following characteristics over a long period of time and to a marked degree that adversely affects a child's educational performance:
- An inability to learn that cannot be explained by intellectual, sensory, or health factors.
- An inability to build or maintain satisfactory interpersonal relationships with peers and teachers.
- Inappropriate types of behavior or feelings under normal circumstances
- A general pervasive mood of unhappiness or depression
- A tendency to develop physical symptoms or fears associated with personal or school problems."
For this category, along with others that we've discussed today, it's important to note that you can't just take the definition as the classification of the child. It really is a team decision with the parents, medical professionals, and the special education teacher all involved.
For example, if a parent said, "Well, my child just seems unhappy, and they're not happy in school" and they happen to see this definition, they might think well, my child should be labeled emotional disturbance and needs special education services. Again, the first step is always the referral, and the team needs to see whether it really is severe enough that the child needs this disability category classification.
Hearing Impairment (HI)
The next category is hearing impairment. A hearing impairment is identified when a student's hearing loss is in the mild to moderate range. Typically, hearing loss below 90 decibels is considered a hearing impairment. Many students in this disability category can be mainstreamed with some assistance. Again, this is below 90 decibels, so they do have some hearing and are able to hear some within the classroom. Students with a hearing impairment might need a hearing aid, cochlear implant, speech therapy or assistive listening devices to assist them. The goal again will be that the child can be in the classroom performing with his peers and just needs some extra support to be successful.
Multiple Disabilities
The category of multiple disabilities is a combination of more than one disability category. You'll typically see multiple disabilities listed alongside other areas in the IEP health section. For example, the student could be identified as having a speech disability, multiple disabilities, and other health impairments. It's important to note that there could be many different disability categories listed in the health area on the IEP. We will take a look at an example of where you would put these disability categories later. Often in this disability category, students will need a variety of supports for all areas of life. This could include help with eating, help with hygiene skills, or help walking in the hallway. There is a wide range of needs in this disability category.
Orthopedic Impairment (OI)
A student will qualify under the category of orthopedic impairment if the child has a severe orthopedic impairment that affects the child's ability to succeed in school. These are more severe impairments that are caused by birth defects, illnesses, or other factors such as injuries. This is not if a child breaks his arm and the ability to succeed is affected only for a short period of time. This category would be assigned only if something more severe was happening with the child.
Students in this category typically need physical and communication supports to be successful in the classroom. An occupational therapist (OT) or a physical therapist (PT) often provide support for the child. Teachers should never be alone in providing all the services for the child. It really is a team effort, even if the OT and PT can't always be with the child. They can always provide support via phone call meetings, emails, or regular correspondence so the teacher feels more supported while they're working on these skills with the student.
Other Health Impairment (OHI)
The IDEA defines other health impairment as "...having limited strength, vitality, or alertness, including a heightened alertness to environmental stimuli, that results in limited alertness with respect to the educational environment that
- Is due to chronic or acute health problems such as asthma, attention deficit disorder or attention deficit hyperactivity disorder, diabetes, epilepsy, a heart condition, hemophilia, lead poisoning, leukemia, nephritis, rheumatic fever, sickle cell anemia, and Tourette syndrome; and
- Adversely affects the child's educational performance."
Qualification for this disability category will occur only if health impairments severely impact the student's education. Again, as we discuss which category a student will qualify for it needs to be severe enough that the child would need additional support. Teachers need to emphasize the point that a student's impairment must be so severe that he or she needs a modification or accommodation to be successful in the classroom. For example, asthma is listed in this definition from the IDEA. That doesn't mean just because a student has asthma, they're going to qualify for this category and they're going to qualify for special education services in the school. The asthma would need to be so severe that they need an alternate classroom environment or additional support for the success of their classroom experience.
Specific Learning Disability (SLD)
A specific learning disability is defined as a disorder in one or more of the basic psychological processes involved in understanding or in using language, spoken or written, that may manifest itself in the imperfect ability to listen, think, speak, read, write, spell, or to do mathematical calculations, including conditions such as perceptual disabilities, brain injury, minimal brain dysfunction, dyslexia, and developmental aphasia. This is typically diagnosed at the elementary school level rather than at a younger age because the team and the teachers are able to see how the student is performing with his or her other peers.
Speech or Language Impairment
The category of speech or language impairment is a communication disorder that adversely affects a child's ability to talk, understand, read, and write. If a student qualifies for speech services at the school level, they might have had an IFSP at a younger age and received speech services. Now at the school-age, it will be listed as a speech or language impairment with an IEP.
As I mentioned, early intervention is key. For example, my son had an IFSP for a speech impairment, but by the age of three, he no longer needed these services. We never got to the IEP level with him getting this category. This disability can be seen in combination with other disability categories on the IEP and you will commonly see on an IEP a child who has a speech or language impairment along with another disability category.
Traumatic Brain Injury (TBI)
A traumatic brain injury occurs when an injury is caused to the brain from an external physical force, such as falls, violence, or a vehicle collision. Unfortunately, some shaken baby syndrome situations, violence in the home with guns, or any type of serious falls can cause a traumatic brain injury. This can be a very challenging situation at times because the child is not typically born with this type of disability. It is sometimes a very sensitive situation with the family and the team. Hereditary brain injuries, degenerative conditions, or injuries caused to the brain by birth complications do not fall under this category and they would be under a different IDEA disability category.
Visual Impairment (VI)
The last IDEA category we'll talk about today is visual impairment. Impairment in vision must be significant enough to impede educational performance. This includes partial sight up to blindness. Some students might have a visual impairment disability, but do have some sight that they're able to use. Assistive technology can significantly improve the classroom experience for these children. A great example is a lightbox. It's just a really bright box with lights coming through it. You can even have the book straight on the lightbox for a reading activity. It brings the focus to the book. You could have tangible items on top of a lightbox as well, which is a great sensory activity.
I know this has been a lot of information and I do encourage you to read more on these 13 IDEA categories, as I only covered the basics of each of these disabilities.
Individualized Education Program
Now we're going to move on to the individualized education program. This is commonly referred to as the IEP in the school system. You'll hear a lot about IEPs, whether you're a general education teacher or a special education teacher. The IEP is a customized plan for school-aged students. Again, the IEP begins the day a child turns three and goes through age 21. It actually stays in effect until the day before the 22nd birthday, so the third birthday up until the 22nd birthday is when students are legally able to have an IEP in effect in the school.
Parents are legally obligated to be a part of all the decision-making procedures with an IEP and should be notified of all assessments taking place. This is a big difference from the IFSP and the 504 plan, which I"ll talk about soon. The IEP requires parents to be notified of all steps along the way. With an IFSP parents are an intricate part, as we discussed, but there's a lot more wiggle room, per se, that they can make changes along the way.
The IEP has certain guidelines that they do need to follow under the IDEA. It is important to keep parents in the loop, just like the IFSP. Quarterly updates are important, so parents know what this child is working on at school. Annual meetings are required. Schools will receive additional funding for a child with an IEP so that they can help get some of the therapists in the school, get extra visual supports, or assistive technology. This is different from the 504 plan we'll talk about next.
The IEP team, including the special education and general education teachers, are accountable for making progress and enhancing student goals. It is important that all educators in the building, whether it's the gym teacher or the special education teacher working with the child, are made aware of the IEP goals and are all working towards those benchmarks.
Another Option
If a student has a significant limitation and does not qualify for an IEP, Section 504 of the Rehabilitation Act might be the best option. This is commonly referred to as the 504 plan or just 504. This plan provides additional support and is protected under the Americans with Disabilities Act (ADA). There are legal guidelines set up, but it does not have the same legal ramifications in the school setting. For example, there are no legal requirements for a written plan or parent involvement. However, it is still important to include the parents along the way. Parents and educators need to advocate for students having a 504 even more so because there are not as many legal ramifications. It's important to make sure that all the services that are discussed are followed through within the school. If the student needs additional time for an activity and that's what was discussed for the 504 plan, then the teacher and the parent need to be sure the child is getting the services and accommodations. As I mentioned before, schools do not receive additional funding for students with 504 plans.
Commonly Used Abbreviations
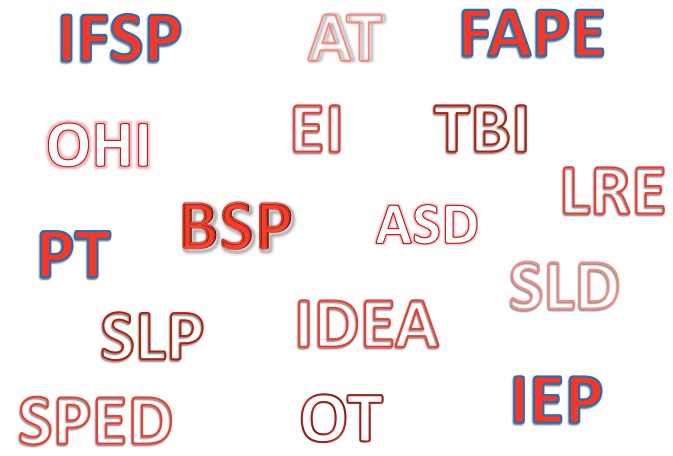
Figure 1. IEP Abbreviations.
As you can see in figure 1, there are many abbreviations and acronyms used daily in the school setting. It can be confusing and unclear, not only to parents but to teachers, too. I've already used some of these today, as you've seen (FAPE, IDEA, IEP, OT). There are so many different abbreviations that teachers use and it is sometimes referred to as alphabet soup. That can be a fun way to lighten up IEP meetings, saying, "Oh we're well aware that this can be confusing at times." There are so many abbreviations and acronyms and we want everyone to be on the same page and be aware of these different abbreviations. I caution you to not use abbreviations too much because the jargon does get confusing for parents during IEP meetings.
- SPED – Special Education
- BSP – Behavior Support Plan
- FAPE – Free Appropriate Public Education
- EI – Early Intervention
- LRE – Least Restrictive Environment
- OT – Occupational Therapy
- PT – Physical Therapy
- SLP – Speech-Language Pathologist
- AT – Assistive Technology
One commonly seen abbreviation is SPED, sometimes referred to as the special education program. You also might see BSP which is a behavior support plan or FAPE which is free appropriate public education. Remember, we discussed FAPE under the IDEA categories. EI stands for early intervention. Sometimes you'll see that used with children with the IFSPs at a younger age. The term least restrictive environment (LRE) is used when you're trying to find the physical environment that is most appropriate for a student.
OT is occupational therapy, PT is physical therapy, and SLP is a speech-language pathologist. AT stands for assistive technology. Assistive technology can include a certain type of technology tool that could be listed as an AT accommodation on an IEP. These terms can make it easier when writing plans or talking about programs, but, as I've mentioned, you do want to be careful that they're not overused to the point where it's a bit confusing.
Understanding the IEP Process
- Referral
- Students can be referred by parents, healthcare professionals, or the special education team.
- Evaluation
- Assessment tools, observation, and data will help determine whether a student qualifies for an IDEA disability category.
- Must have parental permission.
- Eligibility
- If the student is eligible for special education services, the IEP process begins.
- Development of the IEP
- The IEP team will start collaboratively developing the plan.
- The IEP plan must be created thirty days from eligibility determination.
- IEP Meeting
- The teacher will set a meeting date with the parents.
- It is also a requirement to notify the parents at least two times prior to the meeting date.
- The IEP plan is a rough draft until the meeting is complete.
- Meetings can be held by phone with parental permission (not recommended unless necessary)
- Implementation
- The IEP will commence with the needed support.
Referral
Let's talk now about the IEP process. The first step of the many steps in the IEP process is the referral step. The referral is typically where it starts unless you have a student that is coming in with an IFSP that has already been referred. Students can be referred by parents, health care professionals, or someone on the special education team. It's a pretty simple process to fill out a referral. Not everyone who is referred will end up qualifying for an IEP, but if there is concern that there are supports that are needed, it does not hurt to start the referral step.
Evaluation
During the evaluation step, many evaluation tools can be used such as teacher observations, data tracking, or professional assessments by a psychologist or school counselor. It is important to remember that all assessments must be approved by the student's parents. If there's any doubt, I would notify the parents and get consent in writing so that they are aware that there are going to be evaluations conducted on the child.
Eligibility
In the eligibility step, if the student is eligible for special education services, the IEP process begins. If you are at this step you know you're ready for the actual development of the IEP itself.
Development of the IEP
The IEP team will collaboratively develop the plan. The IEP plan must be created within 30 days from eligibility determination. If a student is eligible, it is important to note that you have 30 days to complete the IEP plan.
IEP Meeting
Once the plan has been started in the rough draft phase, the IEP meeting needs to be set. The teacher should find out what works for the parents and set the meeting date with them. Sometimes this can be tricky if you're setting a meeting during the day and you have working parents. Also, it is a requirement to notify the parents at least two times prior to the meeting date. This can be done through phone calls, notes home, or in person. It is important to document these attempts.
Remember, the IEP plan is a rough draft until the meeting is complete. Be sure parents know that the plan is not complete. You don't want them to feel like you came to the meeting with a fully completed plan and they didn't have a part of the decision making about the plan for their child. It is a rough draft until the meeting is complete and everyone has decided on the goals and accommodations for the child. The meeting can be held by phone with parental permission. This isn't recommended, because you want the parent to attend face-to-face to gain that rapport, but if it is needed, a phone call is okay. If you have the meeting by phone you will have the parents sign at a later date.
Implementation
The next step of the process is implementation. The IEP will commence with the needed support and the plan is in place. The responsible parties will now start working on the IEP goals. Now you have the plan and are ready to start working on the goals and put everything into motion that was discussed in the meeting.
Additional Information
Student progress is measured and evaluated based on the determined timelines set in the IEP plan. The IEP team should review goals quarterly and provide updates to the parents. You could be documenting progress towards the goals daily with some type of tracking system, but quarterly you'll put all the results together to share with the team and the parents. The IEP is reviewed and revised annually with the IEP team including the parents. The student should be re-evaluated every three years to determine if services or environments need to be revised.
This is a bigger picture of everything. Every three years of the IEP and the whole program, check to see if the diagnosis and the placements are still appropriate. For example, you might come across a situation where after three years, the student does not need the same level of support or even additional support. Or, the student might need a different type of least restrictive environment that gives more support than they were currently getting.
Some information can stay the same or similar from year to year on the plan, just like when you're meeting annually, but it is important to make each plan unique each year. Just think of it as everyone needs a fresh start every year. You don't want to have everything look the same year to year. There should be significant changes annually with the goals and the present levels. We'll get to those next.
Legal Requirements
I've mentioned the word legal several times today, and it is so important that teachers understand this whole process. It's much bigger than just classroom interventions. An IEP is a legal document and we need to be sure that everything that's put into the IEP is being followed appropriately.
The Individuals With Disability Education Act (IDEA) is a federal law to provide rights to students with disabilities. The IEP plan is a legally binding document mandated by the IDEA. All members of the IEP team and school personnel are responsible for following the plan exactly as it is written. The IEP must be followed by all parties involved or legal ramifications could take place. For example, if a student had an accommodation such as needing extra time on a standardized state-type test and the school did not provide that accommodation, the teacher and school could be in legal trouble. This is not meant to scare anyone, but it really needs to be followed. If you are working with a child that has an IEP, please review it and be sure that you're comfortable with it.
- Under the IDEA, the purpose is stated as …
- “To ensure that all children with disabilities have available to them a free appropriate public education that emphasizes special education and related services designed to meet their unique needs and prepare them for further education, employment, and independent living;
- To ensure that the rights of children with disabilities and their parents are protected;
- To assist States, localities, educational service agencies, and Federal agencies to provide for the education of all children with disabilities; and
- To assess and ensure the effectiveness of efforts to educate children with disabilities.”
With this law, every student has a right to free and appropriate public education and they have the right to have all of the same educational experiences as all children.
What must be included in the IEP?
- Present levels
- Gain rapport with family
- Positives are important!
- Annual goals
- Specific, Measurable, Attainable, Realistic and Timely (SMART)
- Related services
- Accommodations and program modifications
- Include duration of time with general education peers
- State and district testing accommodations
- Approximate timeline of services
- Other considerations (when needed)
- Transition plan – starting at 14 years old
- Extended school year
- Nonacademic services
- Transportation services
Now let's discuss the actual plan, the IEP. There are four sections that I feel are most important to discuss. These include present levels, the goals, related services, and the accommodations and modifications.
Present Levels
In this section about present levels, it's important to showcase the student and include lots of positives. This is a great way to gain rapport with students and families, and of course, everyone wants to hear all the wonderful things the student is doing in school. I often tell teachers to use the sandwich method in this section. To use the sandwich method, start with the bread of the sandwich by sharing an engaging story about the student or something positive that happened in class. You could even share something of interest to the student such as Susie really likes to go to gym class with her peers. The teacher can then move on to the meat of the sandwich and share some of the concerns, whether that's test scores or behaviors that might be negatively impacting the child at school. Then finish up the present level section with other positives and or hopeful recommendations moving forward with the school year.
Annual Goals
If the meeting is not an initial IEP, then the team should discuss the past goals and how the progress was for the year. Use the documentation to develop new annual goals. It is okay to continue the goals from year to year, but it is important to change it in some ways. The student needs to start fresh. Goals should be SMART: specific, measurable, attainable, realistic, and timely. If you're using the same goal year after year, you might realize that a goal is not necessarily attainable or realistic.
Here is an example of a SMART goal.
Susie will identify seven of 10 sight words each week for the first quarter of school.
It's specific because it says exactly what she's expected to do - identify sight words. It's measurable because we want her to identify seven of 10. It's definitely attainable and realistic and it's timely because you want it completed in the first quarter of school and that we're going to be working on that each week.
Related Services
Related services are support services that are required to assist a child with a disability so he or she can benefit from special education. These could include some of those areas we discussed before such as speech therapy, psychological services, physical or occupational therapies, counseling services, and school or health nurse services. I once had a student that needed to be fed throu
