Editor’s note: This text-based course is an edited transcript of the webinar, Inspiratory Muscle Training: A Review of the Evidence, presented by Jessica DeMars, BSc.P.T.
It is recommended that you download the course handout to supplement this text format.
Learning Outcomes
After this course, participants will be able to:
- Describe the benefits and contraindications of IMT
- Discuss how to evaluate and critique the use of IMT in various clinical populations.
- Explain IMT within a cardiorespiratory population
Introduction
I would like to emphasize that my primary role is that of a musculoskeletal physiotherapist, with respiratory physiotherapy being a secondary focus. This distinctive blend of musculo-respiratory expertise forms the foundation of my background. I hope that attendees will gain a comprehensive understanding of initiating inspiratory muscle training (IMT) in their practice.
The majority of my experience with IMT involves working with athletes dealing with milder lung diseases. Despite the increasing evidence supporting the effectiveness of IMT across various respiratory conditions, its widespread adoption remains limited. My aim here is to facilitate the translation of this knowledge and encourage practitioners to delve into the subject, much like I have in several areas.
What Is Inspiratory Muscle Training (IMT)?
When contemplating inspiratory muscle training, the underlying consideration is the potential contribution of inspiratory muscle weakness to shortness of breath or functional limitations. It is important to remember that the diaphragm, being a skeletal muscle, is susceptible to weakness or dysfunction. Thus, it can significantly benefit from targeted strength training.
Identifying respiratory weakness may not be as conspicuous as recognizing, for instance, weakness in the quadriceps that hinders climbing stairs. It does not present itself prominently, except perhaps in certain clinical scenarios. However, this respiratory weakness can manifest in reduced exercise tolerance or exertional shortness of breath. The definition of respiratory muscle weakness lies in diminished muscle contractility, leading to an inability to generate normal pressure and airflow during breathing. Notably, this is not readily apparent without specific testing; it may not be the initial consideration.
In contrast, as a physiotherapist, pinpointing muscle weakness in other areas is often more straightforward. For instance, having someone attempt to walk up a staircase can quickly reveal muscular deficiencies. This lays the groundwork for the historical contemplation of inspiratory muscle training.
Inspiratory muscle testing involves assessing the strength and function of the muscles responsible for inhalation, specifically the muscles that help you breathe in air. It boils down to weight training for the inspiratory muscles. Training these respiratory muscles, particularly the inspiratory ones, necessitates an external load – a specific and targeted resistance. Placing a book on the belly, for instance, does not quite meet the criteria. This testing is often conducted to evaluate respiratory function and can be useful in assessing conditions such as respiratory muscle weakness or dysfunction.
One common method of inspiratory muscle testing is through the use of a device that measures the force generated during inhalation. This information can be valuable in understanding and managing respiratory health. Precision in resistance is key. The primary objective of IMT is to enhance the functionality of respiratory muscles through specialized loading. From my physiotherapist perspective in Canada, where we are commonly referred to as physios, precision is crucial in deriving the benefits of strength training. Numerous studies, a handful of which I will touch upon in this presentation, consistently demonstrate that IMT effectively enhances respiratory muscle strength and endurance. This improvement often translates into a reduction of symptoms and enhanced overall function.
Types of IMT
There are two primary types of inspiratory muscle training methods. The first one is flow-resistive loading. In simple terms, this method obstructs airflow, necessitating an increased force to draw air in. Imagine, for instance, breathing through a straw – if you inhale forcefully, it creates resistance. The smaller the opening, the higher the respiratory load. Some devices offer varying levels of opening. Unfortunately, this method has limitations in terms of measurability. It depends on both the size of the opening and the individual's level of effort. Breathing in slowly through the straw results in minimal resistance, requiring a more substantial effort to generate resistance. It, therefore, tends to be somewhat patient-dependent.
The other widely used and extensively studied type of device is the pressure threshold loading device. In the pressure threshold loading method, generating airflow requires overcoming a pressure load to lift open the valve. This process resembles weightlifting – much like lifting a 10-pound weight- and demands actual effort to initiate movement. Importantly, this method is independent of the breathing rate or the individual's level of effort. Devices employing pressure threshold loading typically offer an adjustable load, making them more measurable. These devices are quantified in centimeters of water, and this measurement can be more accurately calculated based on maximum inspiratory pressure. While flow-resistive devices are generally more affordable and accessible in the general market, pressure threshold devices offer a more precise and measurable approach.
Review of Devices
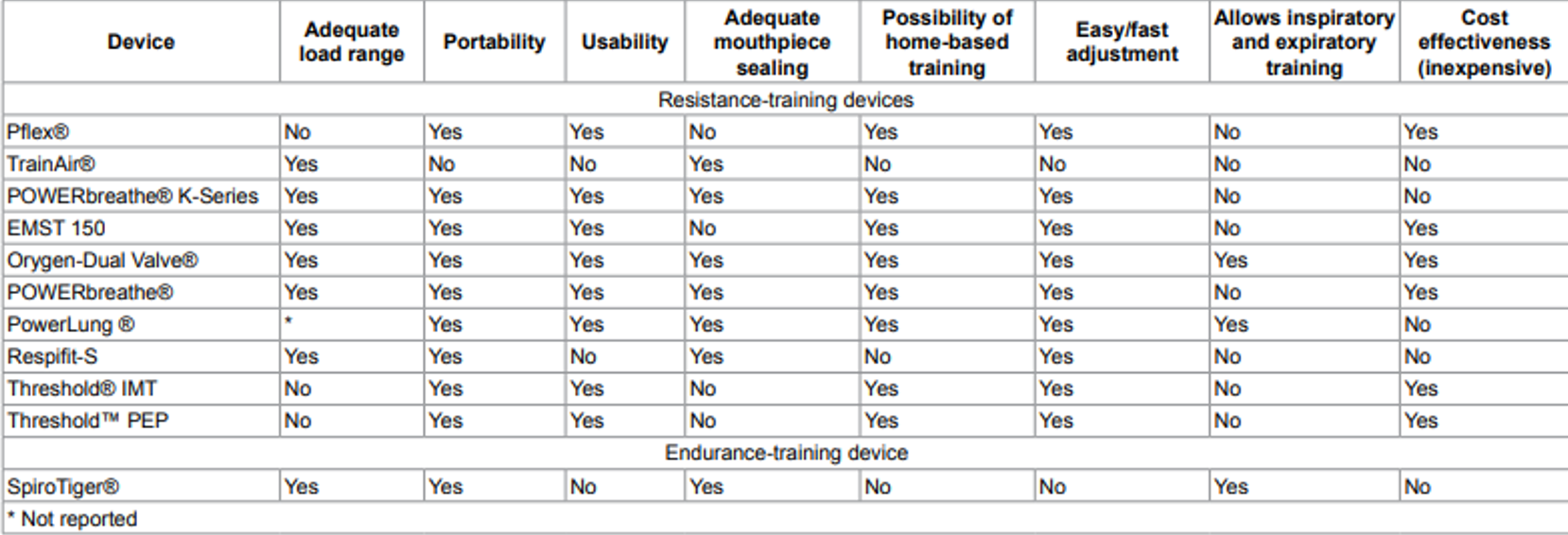
Figure 1. Characteristics of the evaluated respiratory muscle training devices (Menzes et al., 2018, Open Access).
In clinical settings, pressure threshold devices are more commonly used, and the market has seen a proliferation of such devices. This information is based on an article from 2018, and it is worth noting that there may be new devices on the market or ones that are no longer available, like the Phillips threshold device, which is no longer being produced. The Phillips device was widely recognized for being an affordable and straightforward pressure threshold device.
The purpose of this review is to outline the mechanisms and characteristics of various respiratory training devices available at the time, offering valuable insights for those contemplating the integration of IMT into their practice. Examining the table, it is evident that not all devices provide an adequate load range. While the threshold device was accessible in terms of cost, its limited range made it less beneficial for diverse populations. Additionally, some devices lack an ideal mouthpiece, hindering the ability to achieve a proper seal. This aspect is particularly crucial for populations with neuromuscular challenges that may struggle to achieve a secure seal.
Certain devices allow users to create a seal simply by placing them against their mouths. Additionally, there are devices designed for both inspiratory and expiratory training, although previous evidence suggested that simultaneous training for both might not be ideal—favoring a focus on either inspiratory or expiratory training.
It is important to note that some devices may be cost-prohibitive, potentially limiting accessibility for a broader population. Considering these factors is essential when contemplating the implementation of IMT into practice, ensuring that the chosen devices align with the needs and constraints of the intended user base.
Proposed Mechanisms of Benefit
The proposed mechanism behind the benefits of IMT aligns with the principles of strength training applied throughout the body. When a muscle undergoes training, structural changes often occur, and recent advancements, such as real-time ultrasound, allow for the measurement of diaphragm thickness. Increasing thickness and contractility typically signify improved function.
Research, particularly in athletes, reveals that strengthening the diaphragm enhances the respiratory metaboreflex. Some studies demonstrate an increase in oxygen uptake at the lactate threshold or a reduction in lactate buildup. Essentially, this means individuals can exert themselves a bit more strenuously before anaerobic exercise produces a significant buildup of lactate, necessitating a pause. While there is evidence suggesting that IMT can improve lung function, the improvement may stem from the ability to take larger, more forceful breaths and expel air more efficiently.
This differs from addressing changes associated with airway obstruction, as seen in conditions like asthma and COPD. Anecdotal observations and research findings indicate some improvement in pulmonary function, although it is not a cure-all for conditions characterized by airway obstruction.
Metaboreflex
Metaboreflex is a physiological response that comes into play during exercise, particularly in the context of anaerobic exercise. As one engages in physical activity, metabolites such as lactate, potassium, and phosphate accumulate in skeletal muscles. These metabolites are sensed by receptors within the muscles, which then transmit this information to the dorsal horn of the spinal cord through group three and four muscle afferents. From there, the information travels to various areas in the brainstem, including the nucleus tractus solitarius and other cardiovascular control centers, which regulate blood flow and the contraction of skeletal muscles.
This intricate process leads to a series of hemodynamic adjustments. Interestingly, the respiratory muscle metaboreflex is considered even more potent than its counterparts, playing a crucial role in regulating various physiological responses during exercise.
In response to increasing metabolites in the inspiratory muscles during exercise, the metaboreflex is triggered. This reflex prompts a redirection of blood flow and oxygen from the periphery to the respiratory muscles. The rationale behind this response is to prevent fatigue in the respiratory muscles; the body prioritizes ensuring that the respiratory system remains functional. Breathing always takes precedence.
For instance, during high-intensity activities like a time trial on a bike, an individual may experience fatigue in their leg muscles, characterized by a sensation akin to having cement-filled legs due to lactic acid accumulation. However, the body strategically ensures that the respiratory muscles do not reach a point of exhaustion. Preserving the integrity of the respiratory system becomes a priority even when other muscle groups face fatigue.
The metaboreflex, triggered by the accumulation of metabolites, is influenced by IMT. Studies, such as Dempsey et al. (2002), suggest that IMT can effectively delay the onset of this reflex. Using the example of a 40-minute time trial on a bike, if the wall is typically hit at the 30-minute mark, individuals undergoing IMT may experience that challenge closer to the 32 or 33-minute mark. In sports performance, such a shift can have a significant impact.
This observation extends beyond athletics, as research explores the potential impact of the metaboreflex in populations with conditions like COPD. Respiratory muscle weakness and an early onset of the metaboreflex may be contributing factors limiting exercise capacity in these populations. IMT emerges as a potential intervention to address and mitigate these challenges, showcasing its relevance not only in sports performance but also in managing respiratory limitations in various disease states.
Precautions and Contraindications
- A history of spontaneous pneumothorax
- Pulmonary hypertension or large bullae on chest x-ray.
- Marked osteoporosis with a history of rib fractures.
- Desaturation during or following IMT (<94%).
- Asthma patients who have a very low symptom perception and suffer from frequent, severe exacerbations or with an abnormally low perception of dyspnea
- If a patient is suffering from a ruptured eardrum or any other condition of the ear
- Patients with marked elevated left ventricular end-diastolic volume and pressure
- Patients with worsening heart failure signs and symptoms after RMT / IMT
- Active cold, sinusitis, or respiratory tract infection
When considering IMT, it is crucial to be mindful of potential precautions and contraindications, many of which are rooted in the theoretical possibility of generating significant negative pressure swings during training. As individuals draw in a breath, the pressure changes can pose certain risks.
For instance, caution should be exercised if a person has a history of spontaneous pneumothorax or presents with large bullae on a chest x-ray. In such cases, creating intense pressure within the lungs may not be advisable. Similarly, individuals with severe osteoporosis and a history of rib fractures should approach IMT cautiously. The aggressive inhalation involved in the training process may pose risks, especially if individuals experience desaturation during its application. These considerations underscore the importance of tailoring IMT interventions based on an individual's specific medical history and condition.
In the realm of precautions, it is noteworthy to exercise caution with asthma patients who have very low symptom perception and experience frequent severe exacerbations. Additionally, individuals with an active cold, sinus or respiratory infection, or an eardrum issue should approach IMT with care, as the negative pressure generated during training may not be beneficial in these conditions.
When it comes to osteoporosis, it is not necessarily a contraindication but a precaution. In such cases, the approach to IMT may involve adjusting the load and repetitions. Opting for lower loads and longer repetitions could be a more prudent strategy, akin to modifying strength training in any other context. The key takeaway is the importance of tailoring the IMT approach based on individual characteristics and conditions, emphasizing a personalized and cautious prescription. This ensures that the potential benefits of IMT are realized while minimizing any associated risks.
Using IMT in Clinical Populations - What is the Evidence?
When to Consider IMT?
- Symptoms present that might be associated with respiratory muscle weakness, or there is an increased load on the pump:
- Exertional or ‘positional’ dyspnea, impaired cough, ventilatory failure/hypercapnia
- Patients at risk for respiratory muscle weakness:
- COPD/CHF/ICU
- Neurological diseases (MS, Parkinson's, CVA, diaphragm paresis)
- Neuromuscular disease
- Patients with an increased load on the respiratory system
- Reduced chest wall compliance: kyphoscoliosis
- Reduced lung compliance: lung fibrosis
- Patients after prolonged mechanical ventilation and weaning failure
In exploring the application of IMT in clinical populations, we will delve into some of the evidence. It is worth noting that the scope here is not exhaustive, given the intricate nature of IMT and its impact across diverse clinical scenarios. The increasing focus on respiratory muscle weakness and its implications in various clinical settings has spurred a wealth of research and interest in understanding the efficacy of IMT for specific populations. The ongoing research and the expanding interest in this domain emphasize the significance of evaluating its potential applications in different contexts.
The selection of populations for IMT consideration hinges on the underlying rationale for incorporating this training. For those keen on a more in-depth exploration, Rik Gosselink, a physiotherapist, has dedicated considerable time to studying IMT. His extensive research and literature offer insights into the benefits of IMT and guide the process of selecting patient populations suitable for this intervention. This information is drawn from a presentation he gave at the Australia Physiotherapy Association. It serves as an excellent summary of the considerations for inspiratory muscle training. Although the slides are not available for viewing, the details can be accessed online, Research Group for Rehabilitation in Internal Disorders.
Symptoms play a pivotal role in deciding when to incorporate inspiratory muscle training. The presence of symptoms potentially linked to respiratory muscle weakness, such as exertional or positional breathlessness, an impaired cough, or indications of ventilatory failure, suggests a scenario where IMT might be beneficial. Another consideration arises when there is an increased load on the respiratory pump, prompting the thought that reinforcing respiratory muscles could be advantageous.
Patients at risk for respiratory muscle weakness, including those with COPD, heart failure, and those who have undergone ICU treatment, present situations where IMT might be particularly relevant. The subsequent discussion will further delve into the implications of IMT in ICU settings. Neurological diseases are certainly a focus, along with neuromuscular diseases and patients experiencing an elevated respiratory system load. This could manifest as reduced chest wall or lung compliance, and it is especially pertinent in patients who have undergone prolonged mechanical ventilation and experienced weaning failure. The ongoing research in this area is quite compelling. A recent study by Lista-Pax et al. (2023) aimed to define when we should consider inspiratory muscle weakness. It could be a valuable reference to have on hand, even though my colleagues and I playfully jest about the idea of having the reference equation readily available for mental calculations.
Methodology (Lista-Pax et al., 2023)
- Measurements Plmax/PEmax
- SEPAR protocol in agreement with ATS/ERS guidelines
- Flanged mouthpiece
- Pressures sustained 3-5 sec
- Min 6 acceptable manoeuvres, 3 of them with variability <5%
- SEPAR protocol in agreement with ATS/ERS guidelines
Results
- Reference equations
- PImax= 61.48 + 0.66 * age + 1.55 * BMI - 0.01* age2
- PImax= 98.60 + 1.18 * age + 0.76 * BMI - 0.02 * age2
- PEmax= 74.75 + 1.67 * age + 1.75 * BMI - 0.02 * age2
- PEmax= 58.11 + 3.71 * age + 2.64 * BMI - 0.04 * age2
- Cut-offs
- Inspiratory muscle weakness
- Female 62 cmH20
- Male 83 cmH20
- Expiratory muscle weakness
- Female 81 cmH20
- Male 109 cmH20
- Inspiratory muscle weakness
Examining the work of Lista-Pax et al. (2023) adds a layer of complexity to our understanding. The study encompassed a sizable sample of 610 individuals, spanning the wide age range of 18 to 80 years. While the substantial sample size is commendable, the broad age spectrum introduces a challenge, given the potential physiological variations across such a diverse population. The study's key findings provide cutoff values for inspiratory and expiratory muscle weakness. In women, inspiratory muscle weakness is identified below 62 centimeters of water, while in men, the cutoff is 83 centimeters of water. For expiratory muscle weakness, the respective cutoffs are 81 centimeters of water for women and 109 centimeters of water for men. Falling below these thresholds indicates the presence of muscle weakness. It is worth noting that these findings contribute valuable insights, particularly for clinicians working with individuals exhibiting respiratory muscle weaknesses. However, the application of inspiratory muscle training may vary across different healthcare practices. Internationally, physiotherapy colleagues specializing in breathing pattern disorders may adopt unique approaches to inspiratory muscle training, reflecting the diversity in clinical methodologies within the field.
When assessing the impact of diaphragm weakness, our approach differs from setting a rigid cutoff, such as the thresholds mentioned in previous studies. Rather than solely relying on specific numerical values, we consider functional weakness. This means that even if an individual's maximal inspiratory pressure exceeds the defined cutoffs, we still evaluate factors like endurance and performance in real-life situations. For instance, if someone experiences breathlessness during an activity requiring significant core activation and body movement, we may consider IMT even before reaching the defined cutoff levels. Our practice takes into account symptoms and functional limitations alongside objective measurements. If an individual falls below their maximum respiratory pressure and exhibits breathlessness during certain activities, we might initiate IMT earlier, prioritizing the improvement of diaphragmatic function and strength.
Prior to the recent study (Lista-Pax et al., 2023), our reference point was a 2013 study that provided some insight into maximum respiratory pressures. However, the information available in the literature on this topic has been somewhat limited. The 2013 study by Sclauser Pessoa et al., while informative, lacked detailed categorization by age and gender. In contrast, the current study offers a more nuanced breakdown, allowing us to consider age-specific variations. For example, a 30-year-old athlete with a maximum inspiratory pressure of 90 centimeters of water might surpass the general cutoff but would still be identified as someone to work with to enhance diaphragmatic function and strength. This nuanced approach acknowledges the variability in respiratory capabilities across different age groups and genders, enabling a more personalized and effective intervention strategy.
COPD
Let's delve into various population groups, particularly focusing on COPD. This area is intriguing due to the diverse evidence available. The rationale for considering it lies in the fact that hyperinflation can lead to diminished diaphragm function and reduced diaphragm thickness. Notably, a decline in inspiratory muscle strength in COPD was observed as early as 1996 by Gosselink et al.
To illustrate the evolution of studies on this topic, Gosselink et al. (2011) findings indicated that inspiratory muscle training enhances not only inspiratory muscle strength and endurance but also functional exercise capacity, dyspnea, and overall quality of life. However, by 2018 (Schultz et al.), a different perspective emerged, suggesting that three weeks of inspiratory muscle training added to pulmonary rehab enhances inspiratory muscle strengthening. Nevertheless, this addition does not result in improvements in exercise capacity, quality of life, and dyspnea. In summary, the evidence surrounding hyperinflation's impact on COPD and the efficacy of inspiratory muscle training is diverse and has evolved over the years. From initial studies showing improvements in various parameters to recent findings indicating specific limitations, the landscape of knowledge in this area is complex.
I would argue that drawing solid conclusions from a mere three weeks of any intervention, particularly in the realm of exercise, might be overly optimistic—an opinion shared by many. Assessing the efficacy of a practice based on only two measures before and after such a short duration may not offer sufficient insight, potentially explaining the lack of observable functional translation.
However, in 2023, Ichiba et al. completed a study involving a more extended period of inspiratory muscle training—spanning two months at 50% of maximum inspiratory pressure—which yielded more encouraging outcomes. This intervention not only improved maximum inspiratory pressure (MIP), diaphragm thickness, and the six-minute walk test but also led to a reduction in dyspnea and leg fatigue. Once again, the outcomes appear varied, prompting a closer examination of the studies to discern the nuances of how the intervention is implemented.
In 2010, Simms et al. conducted a study at the University of Toronto in Canada, aiming to enhance inspiratory muscle implementation. The research presented a nuanced journey marked by both successes and challenges. Upon inspecting the table's data, a distinct pattern emerges. In 1992, the study concluded that IMT lacked effectiveness in treating COPD. However, a pivotal shift occurred in 2002 when IMT alone exhibited a substantial positive impact on inspiratory muscle strength, endurance, and the mitigation of dyspnea both at rest and during exercise.
The narrative took a downturn in 2003, with a declaration of insufficient evidence to endorse the use of IMT in COPD, prompting a call for additional studies. By 2005, a reversal of fortune is evident, showcasing significant improvements in inspiratory muscle strength and endurance. This positive trajectory is reiterated later in the same year. In 2006, the study recommended considering IMT as a potential therapeutic approach, particularly for patients displaying signs of respiratory muscle weakness.
In 2007, the updated Canadian Thoracic Society Guidelines did not include any mention of IMT. The subsequent year, a systematic review in 2008 revealed enhanced outcomes in exercise capacity and a measure of quality of life, though the clinical significance remained unclear. Concurrently in 2008, there were notable advancements reported.
The trajectory continued with a series of significant improvements, reflecting a fluctuating pattern. Despite these positive findings, the practical implementation of IMT remained elusive. This paper advocated for the use of IMT in the population, lamenting the apparent lack of adoption. Even after two decades, the beneficial aspects highlighted in studies were not universally embraced by the respiratory population. Despite the demonstrated benefits and minimal side effects, IMT continues to face resistance in gaining traction within the respiratory community. The potential for positive outcomes persists, yet widespread acceptance appears to be elusive.
Exploring IMT is a worthwhile endeavor, especially when considering its potential application for patients with COPD. A valuable resource in this context is a practical guide from Hill et al. (2010) that delineates the clinical rationale for its utilization. The guide recommends considering IMT for individuals unable to fully engage in whole-body exercise due to various comorbid conditions. This perspective prompts the consideration of IMT not only as a targeted intervention but also as a potential pre-habilitation strategy. For instance, if a patient finds whole-body exercise challenging or feels too breathless to participate, IMT could serve as an initial step. By focusing on strengthening respiratory muscles, IMT lays the foundation for improved core stability, facilitating progress in overall exercise capacity. This dual approach addresses both respiratory challenges and broader physical conditioning, offering a comprehensive strategy for enhancing patient engagement in exercise programs.
Continuing the exploration of IMT as an adjunct, it is essential to adhere to specific recommendations outlined in the guide. Exclusion criteria involve individuals at risk for spontaneous pneumothorax or rib fractures. Supervision during training is crucial, including the monitoring of respiratory rate and oxygen saturation, aligning with common sense safety precautions. The assessment process, both before and after an IMT program, involves measuring maximum respiratory pressure, dyspnea levels, quality of life, and exercise capacity. This systematic evaluation aims to discern the impact of IMT on individual patient outcomes, contributing to a tailored training program.
Guidelines advocate for the use of pressure threshold training devices, emphasizing their accuracy. Interval-based training programs are recommended, with loads exceeding 30% of the MIP, progressing based on perceived exertion. Implementing IMT is not just about the initial gains in strength; it necessitates a sustained effort through a maintenance program. Strength gains are evident initially, but a consistent approach is required to ensure long-term benefits. For healthcare professionals considering IMT in COPD management, this resource serves as a valuable guide, providing comprehensive insights into implementation principles and exercise strategies.
Asthma
- RCT (IMT vs. sham) of 38 participants found improvements in respiratory muscle strength, exercise capacity, quality of life, daily living activities, reduced perception of dyspnea, and fatigue (Duruturk et al., 2018).
- 2023 systematic review and meta-analysis concluded that IMT causes a significant increase in MIP; more evidence is needed to clarify the effect of IMT on respiratory muscle endurance, rescue medication, exercise capacity, healthcare use, and HRQoL (Lista-Paz et al., 2023).
When considering the asthma population, the evidence surrounding IMT appears somewhat mixed. From a clinical perspective, an increase in maximum inspiratory pressure may be observed, but its translation into functional improvement or enhanced quality of life is uncertain. In practical terms, issues related to breathing pattern disorders in asthma seem more prevalent than actual respiratory muscle weakness, based on clinical experience.
IMT may find utility in addressing breathing pattern disorders by providing a resistance that facilitates biofeedback. It can serve as a tool to enhance awareness of proper muscle engagement during breathing. In the athletic context, IMT might be employed to derive performance benefits or to address exercise-induced laryngeal obstruction or vocal cord dysfunction in athletes with asthma.
However, IMT may not be a routine or go-to option for individuals with asthma in day-to-day clinical practice. The research seems to align with this perspective, suggesting that respiratory muscle weakness is not a predominant feature associated with asthma. Thus, the decision to incorporate IMT into asthma management may be contingent on specific clinical considerations, including the presence of breathing pattern disorders or specific performance goals for athletes with asthma.
Restrictive
- 8 weeks of IMT added to PR improved inspiratory muscle strength, 6MWD, QOL, and dyspnea (Zaki et al., 2022).
- Systematic review of IMT in ILD suggests there is a positive effect of IMT on respiratory muscle function, quality of life, exercise capacity, and dyspnea. However, research is still emerging, and existing study designs are of lower quality (Hoffman et al., 2021).
- Decreased MIP and endurance were related to decreased exercise tolerance in sarcoidosis (Marcellis et al., 2013).
- However, weakness tends to be variable in this population.
There's a growing interest in exploring IMT for individuals with restrictive lung diseases, and it seems to be a promising avenue for potential benefits. In conditions characterized by increased respiratory drive but reduced lung compliance, such as restrictive diseases, the mismatch between demand and the ability to generate required pressures becomes apparent. This creates a scenario where strengthening the respiratory muscles could potentially address the challenges posed by decreased lung compliance.
Approaching IMT on an individual basis rather than a population level is emphasized. Assessing whether a person exhibits signs of respiratory muscle weakness and gauging their potential compliance with a training regimen are crucial considerations. The decision to implement IMT should be tailored to the specific needs and characteristics of the individual.
From a physiotherapist's standpoint, evaluating the rib cage's flexibility and pliability is highlighted. A stiff and non-pliable rib cage may necessitate increased effort from respiratory muscles to achieve expansion and facilitate adequate inspiratory volumes. This mechanical perspective underscores the rationale behind considering IMT for individuals with restrictive lung diseases.
I think this is an area where we could see more increased research focus on inspiratory muscle training, particularly within the context of restrictive diseases. The mechanical reasoning behind its potential benefits makes it a compelling area for further exploration and investigation.
ICU
Allow me to delve into this topic, bearing in mind that I am not an ICU physiotherapist. Back in my student days, I had some exposure to acute care, though not extensively in the ICU. I hope to capture your interest in this matter. If anyone has experience with IMT in the ICU, I would appreciate engaging in a discussion about it. To me, it seems like a straightforward concept.
We are familiar with PICS (Post-Intensive Care Syndrome) or ICU-acquired weakness. It logically follows that the diaphragm weakens after prolonged ventilation. Approximately one-third of adult ICU patients ventilated for seven or more days exhibit impaired inspiratory muscle endurance or diaphragm atrophy (Bissett et al., 2015). In a 2018 meta-analysis by Vorona et al., IMT emerged as feasible and well-tolerated in critically ill patients, linked to shorter ventilation and weaning periods. The recommended protocol for this population involves high intensity, at least 50%, and low repetitions (Bissett et al., 2020).
If you are considering exploring this further, Australian physiotherapist Bernie Bissett has researched and applied IMT in the ICU, providing a practical guide for clinicians. You can find it referenced at the end of the slide handout and available online. There is a notable movement to champion inspiratory muscle training because it aligns with the recognized weakness in patients, which can complicate the weaning process.
As part of that guide, Inspiratory Muscle Training for Intensive Care Patients: A Multidisciplinary Practical Guide (Bissett et al., 2019) outlines considerations for IMT. For patients who are ventilator-dependent, alert, cooperative, and able to trigger spontaneous breaths with a respiratory rate of less than 25, incorporating inspiratory muscle training is advisable. This helps in initiating diaphragm training for those recently weaned from ventilation.
Being alert and cooperative involves the ability to maintain a lip seal around the mouthpiece or follow the guidelines depicted in the diagram. Considerations for strengthening the diaphragm and aiding in weaning or post-ventilation progression are crucial. This aspect forms a substantial area for contemplation in inspiratory muscle training. The application of IMT extends to various populations. I could have easily expanded this discussion with additional slides due to the abundance of information and diverse perspectives on inspiratory muscle training.
Other Populations
Several studies suggest that preoperative IMT may mitigate the risk of postoperative complications, such as pneumonia and atelectasis, particularly in thoracic surgeries (Karanfil & Moeller, 2018). The growing trend is the integration of IMT as a pre-surgical measure. The objective is to bolster muscle strength, focusing on the diaphragm and inspiratory muscles, thereby minimizing the likelihood of post-op complications. This approach has shown positive outcomes in reducing respiratory complications after stroke, as highlighted in a systematic review of five studies (Menezes et al., 2016). However, one challenge lies in achieving a secure mouth seal, with certain devices facilitating this by allowing the mouthpiece to be placed against the lips.
In a pilot study conducted by Human & Morrow (2021), inspiratory muscle training in children and teens with neuromuscular disease was deemed safe, feasible, and acceptable. The intervention correlated with enhanced inspiratory muscle strength, as well as improved upper limb function and coordination, opening up another avenue for exploration. A fascinating tangent in the realm of physiotherapy explores how inspiratory muscle fatigue alters postural strategies. Lotte Janssens, a physiotherapist, delved into this area in her doctoral thesis, available online in PDF format. Her series of studies examined the role of inspiratory muscles in postural control and how fatigue might impact postural control, extending these findings to individuals with chronic obstructive pulmonary disease (COPD).
The work of Janssens et al. (2015) reveals that respiratory muscle fatigue can influence balance issues in COPD, expanding our understanding beyond the traditional respiratory benefits of IMT. The study observed alterations in postural strategies during unexpected movements, typically measured by placing participants on a movable plate. Individuals with inspiratory muscle fatigue exhibited a greater tendency to adopt an ankle strategy instead of the usual back strategy, a pattern commonly seen in those with low back pain. This insight underscores a connection between low back pain, reduced balance, respiratory muscle weakness, and fatigue. The findings suggest a potential avenue for addressing balance and proprioceptive challenges through targeted inspiratory muscle interventions.
Enhancing diaphragmatic strength and function can lead to improvements in postural strategies and balance. This becomes particularly crucial when addressing the observed reduction in balance among individuals with COPD. Consequently, we must explore whether respiratory muscle dysfunction contributes to this imbalance and whether inspiratory muscle training can bring about positive changes beyond respiratory outcomes, potentially influencing balance and proprioceptive strategies and thereby reducing the risk of falls.
Expanding our perspective on inspiratory muscle training, there is a noteworthy study out of Colorado that gained attention for its focus on inspiratory muscle training in sleep apnea. Despite the initial intent, the randomized control, double-blind study involving 36 adults revealed unexpected benefits: inspiratory muscle training not only lowered blood pressure but also improved endothelial function (Craighead et al., 2021). This finding emphasizes the potential broader impacts of inspiratory muscle training, demonstrating its capacity to reduce blood pressure with just five minutes of daily breathing exercises.
Considering the connection between inspiratory muscle training and diaphragmatic breathing, it is worth investigating how these practices compare in terms of changes in blood pressure. Engaging in diaphragmatic breathing, tied to the parasympathetic nervous system and the vagus nerve, typically leads to lowered heart rate and blood pressure. Exploring whether inspiratory muscle training and diaphragmatic breathing yield similar effects on blood pressure could provide valuable insights.
In conclusion, the multifaceted benefits of inspiratory muscle training extend beyond respiratory improvements, encompassing aspects of balance, blood pressure regulation, and its potential impact on obesity-related respiratory challenges. Further research is warranted to delve deeper into these areas and compare the effectiveness of inspiratory muscle training with other therapeutic interventions, such as diaphragmatic breathing.
Obesity
- Obesity can cause impairments to chest wall mechanics, reductions in lung volumes, and increased work of breathing (Severin et al., 2019)
- Respiratory muscle fatigue is higher in obese individuals with poor sleep quality (Severin et al., 2021)
- Patients with obesity demonstrate respiratory muscle fatigue after peak aerobic exercise ((Severin et al., 2022)
- 2023 systemic review determined that IMT improves physical capacity and IM strength (Caicedo-Trujillo et al., 2023)
Turning our attention to obesity, it emerges as an emerging area of interest in the context of inspiratory muscle training. Obesity induces impairments in chest wall mechanics, reductions in lung volumes, and increased work of breathing. Respiratory muscle fatigue is notably higher in obese individuals with poor sleep quality, and those with obesity display respiratory muscle fatigue after peak aerobic exercise.
Recent findings indicate that individuals with obesity may experience potentially abnormal respiratory muscle fatigue compared to those without obesity. A systematic review from 2023 underscores the positive impact of inspiratory muscle training on physical capacity and inspiratory muscle strength. This intervention is not only easy to implement and relatively inexpensive but also holds promise as an accessible option, particularly for individuals for whom exercise may present challenges. It becomes a potentially empowering self-directed approach, offering positive gains in physical well-being. This is particularly relevant for populations facing barriers to traditional exercise methods.
In considering the diverse range of populations that might benefit from inspiratory muscle training, it becomes apparent that this intervention has far-reaching implications. Its easy implementation and potential positive outcomes make it a valuable consideration across various patient populations. The ever-growing list of potential beneficiaries underscores the versatility and broad applicability of inspiratory muscle training in improving both respiratory and overall physical health.
More?
- GERD
- Sport Performance
- Post COVID (CAREFULLY!)
- Heart Failure
Fascinating research has explored the relationship between reflux and diaphragm strength, highlighting that diaphragmatic strength can influence the tone of the lower esophageal sphincter. The lower esophageal sphincter, situated within the diaphragm, is shown to be affected by the strength or tone of the diaphragm, influencing its closure and pressure. IMT has been investigated as a potential means to improve gastroesophageal reflux disease (GERD). Anecdotal evidence, supported by patient reports, suggests that reflux symptoms may improve with IMT, although caution is advised as excessively high loads during training may exacerbate reflux.
In the realm of sports performance, numerous studies have explored IMT as an ergogenic aid. The potential benefits lie in delaying the onset of fatigue, allowing athletes to push their limits further. This avenue is gaining interest, and it would not be surprising if it starts appearing in social media discussions related to inspiratory muscle training for enhanced sports performance.
A noteworthy area of exploration is the use of IMT in the post-COVID context. While some evidence suggests its potential utility, there is a crucial need for caution, particularly in individuals with post-exertional malaise—a common symptom in those with long COVID. Given that IMT essentially involves exercise, its application in this population requires careful consideration of individual circumstances, such as the presence of respiratory muscle weakness without post-exertional malaise.
Heart failure has also been a subject of recent study, with emerging evidence suggesting potential benefits of IMT. Additionally, ongoing research in the area of double lung transplant recovery is anticipated, as some researchers are delving into the application of IMT post-transplant.
Lastly, a new study has delved into the realm of low back pain. This could be particularly intriguing for physiotherapists as it aligns with their focus. The diverse applications of IMT across various conditions underscore its versatility, providing potential benefits in areas ranging from respiratory health to sports performance and beyond. Depending on the patient population and healthcare setting, these applications may offer relevant and valuable interventions.
Training Protocol
- Research based on quantity – 30 breaths, 2x/day, approximately 40% MIP
- Some studies will advocate for higher loads
- Clinical experience
- Quality vs. quantity
- Aim for pattern first
- Strength vs. Speed
When it comes to training protocols for IMT, existing research often supports a regimen of 30 breaths twice a day, with the load set at approximately 40-60% of the maximum inspiratory pressure. However, it is important to note that some studies advocate for higher loads, and the choice depends on the specific population being addressed. For instance, in the case of COPD, there is a recognition that these individuals possess good endurance in their diaphragm, albeit with reduced power. As a result, a higher load may be more beneficial for COPD patients, focusing on generating the necessary force for activities that demand increased respiratory effort.
Clinical considerations also play a role, especially in fields like breathing pattern disorders. Emphasis is often placed on achieving the most efficient breathing pattern, typically favoring diaphragmatic breathing when all components are functioning optimally. In this context, the goal may be to prioritize quality over quantity in training. It becomes crucial to steer away from training individuals to rely on accessory muscles, except in specific patient populations.
Deciding between strength and speed is another aspect to consider. For certain patient populations, particularly those with upper airway dysfunction, the emphasis may be on speed of breath. Athletes, for instance, might benefit from focusing on breath speed to address upper airway issues related to the pace of breathing. This consideration, however, may not be as relevant in all patient populations and may need to be tailored based on individual needs and goals. The key is to customize the training approach to the specific requirements of the population being addressed.
Is How You Cue Important?
The importance of how you cue individuals during inspiratory muscle training depends on the specific goals and characteristics of the population you're working with. In scenarios where the primary goal is ventilation, such as in the ICU or with patients experiencing diaphragm paralysis, the focus may be on engaging any available muscles for inspiration. In these cases, you prioritize ventilation over the specific muscles involved. Additionally, for patients with pectus excavatum (a condition involving chest wall deformities), high-load diaphragmatic inspiratory muscle training might not be suitable, as it could exacerbate negative pressure and draw everything inward. In such cases, alternative approaches, like practicing with hands behind the head and adopting more of a chest pattern, may be more appropriate.
Cueing becomes crucial in these situations, tailored to the individual's needs and circumstances. A study in 2016 by Ramsook et al. compared the effects of different cueing strategies on healthy men. The study found that diaphragmatic-targeted cueing led to a significant increase in electromyography (EMG) activity of the diaphragm, increased transdiaphragmatic pressure, and decreased scalene muscle activity.
- Found that training with tapered flow resistive loading or pressure threshold loading from Functional Residual Capacity improved respiratory muscle function at higher lung volumes
- Pressure threshold loading from residual volume (standard protocol) restricted gains at lower lung volumes (Van Hollebeke et al., 2020)
Another aspect to consider is lung volume during inspiratory muscle training. Research has explored whether it is better to start from the end of expiration and then breathe in or to follow a regular inhale-exhale pattern. A study by Van Hollebeke et al. compared tapered flow resistive (electronic devices) and standard manual pressure threshold devices and found that better muscle function was observed when starting from functional residual capacity (end exhale) rather than almost reserve volume.
Using a Personalized Approach
- Consider training load (Ren-J S et al., 2021)
- Strength vs endurance
- “task failure”
- Concurrent training – training with activity
- Lung volumes
- Expiratory muscle training…
Being specific in how you cue individuals during inspiratory muscle training can have a significant impact on outcomes, including muscle engagement and function. Tailoring your approach based on individual characteristics, goals, and potential limitations is crucial for effective and safe training. Are you prioritizing strength or endurance? Is the focus on enhancing ventilation, particularly in patient populations like the ICU or those with spinal cord injuries? Perhaps the goal is to improve breathing patterns. I specifically emphasize diaphragmatic breathing, using it as a biofeedback tool. For instance, I might introduce a straw, aiming for subtle adjustments, or opt for a more functional approach, incorporating movement while breathing. This is crucial to address potential issues like breath-holding during activity, ensuring an integrated approach to core stability, breathing, and movement.
Creativity plays a key role in tailoring interventions. Introducing devices during training sessions, where individuals move while breathing, can be effective. The concern here is addressing potential breath-holding habits during activity, especially when there's a need to integrate core stability, breathing, and movement seamlessly.
The ellipsis after "expiratory muscle training" alludes to a distinct and evolving area of research. The focus shifts to different muscles with unique benefits. Determining if a patient would benefit from expiratory muscle training is a topic for another day, yet it highlights the importance of a personalized approach in treatment decisions.
In conclusion, a personalized approach is fundamental to all aspects of treatment. Whether considering strength, endurance, ventilation, or breathing patterns, tailoring interventions to individual needs is key. The evolving nature of research, as seen in expiratory muscle training, further underscores the need for adaptability and personalized care. It seems I've managed to navigate this discussion within the allotted time. If you have further questions or need clarification, feel free to ask.
Questions and Answers
Would it be reasonable to expect stronger voluntary cough reflex in COPD patients?
If your concern is coughing, then directing attention to expiratory muscle training may be beneficial. Improved inspiratory effort, resulting from effective inspiratory muscle training, may enhance expiratory effort as well. This improvement is attributed to a larger lung volume, supporting increased pressure generation for exhalation. When individuals seem to be taking in limited air, inspiratory muscle training becomes a potential avenue for addressing this concern. Moreover, it is noteworthy that inspiratory muscle training might contribute to improved mucus clearance facilitated by the adoption of deeper and more substantial breaths.
The active cycle of breathing, coupled with the use of the inspiratory muscle trainer followed by the positive expiratory pressure (PEP) device, can be an effective strategy for mucus clearance. This approach is particularly noteworthy in the case of emphysema, where the individual finds value in incorporating both devices. The combination of inspiratory muscle training and the PEP device is perceived as beneficial, aiding in the movement and clearance of mucus. This underscores the versatility and individualized nature of respiratory therapy interventions.
What is the major difference between IMT and EMT?
If the primary focus is on enhancing cough, then directing attention to expiratory muscle training becomes crucial. This type of training primarily targets abdominal muscles, offering improvements not only in the abdominal region but also extending benefits to some of the throat muscles. If optimizing cough effectiveness is the goal, expiratory muscle training would be the more targeted and relevant approach in this context.
- IMT Focus: Primarily targets the muscles involved in inhalation or inspiration.
- Purpose: Aims to strengthen and improve the endurance of the muscles responsible for expanding the lungs during inhalation.
- Training Devices: Involves exercises and devices that provide resistance during inhalation, such as inspiratory muscle trainers.
- EMT Focus: Primarily targets the muscles involved in exhalation or expiration, including abdominal and throat muscles.
- Purpose: Aims to strengthen and enhance the endurance of muscles responsible for compressing the lungs and facilitating exhalation.
- Training Devices: Involves exercises and devices that provide resistance during exhalation, often focusing on abdominal muscle engagement
What method would you use, possibly without a device?
When considering alternatives to specialized devices for inspiratory muscle training, simple and cost-effective methods can still offer benefits. For instance, using a book on the belly or incorporating a straw may not provide the same specificity in terms of strength gains, but they can serve as effective tools for training diaphragmatic breathing. Adding a thick elastic band, akin to what's commonly known as a THERABAND in physio, around the lower ribs can introduce an element of resistance. While this may offer more of a biofeedback effect than explicit strengthening, it remains a viable option, especially for those with budget constraints.
Considering the affordability factor, a metal straw and a piece of theraband could be a more accessible solution, providing some resistance and yielding noticeable benefits. Although these makeshift methods may not be as specialized or targeted as dedicated devices, they can still contribute to improving inspiratory muscle function, making them a practical alternative for individuals with financial constraints.
References
Select references are listed here (frequently quoted). A complete reference list is provided in the course handout.
Sclauser Pessoa, et al. (2014). Reference values for maximal inspiratory pressure: a systematic review. Canadian Respiratory Journal, 21(1), 43-50.
Gosselink, R., et al. (2011). Impact of inspiratory muscle training in patients with COPD: what is the evidence? European Respiratory Journal, 37(416-425).
Schultz, K., Jelusic, D., Wittmann, M., et al. (2018). Inspiratory muscle training does not improve clinical outcomes in 3-week COPD rehabilitation: results from a randomised controlled trial. European Respiratory Journal, 51(1702000).
Dempsey, J et al. (2002). Respiratory influences on sympathetic vasomotor outflow in humans. Respiratory Physiology & Neurobiology, Volume 130, Issue 1, Pages 3-20, ISSN 1569-9048.
Ichiba, T., Miyagawa, T., Tsuda, T., Kera, T., & Yasuda, O. (2023). Changes in diaphragm thickness and 6-min walking distance improvement after inspiratory muscle training in patients with chronic obstructive pulmonary disease: Clinical trial. Heliyon, 9(9), e20079.
Simms, A. L., Li, L. C., & Reid, W. D. (2011). Development of a theory-based intervention to increase prescription of inspiratory muscle training by health professionals in the management of people with chronic obstructive pulmonary disease. Physiotherapy Canada, 63(3), 315–323.
Hill, K., et al. (2010). Inspiratory Muscle Training for Patients with Chronic Obstructive Pulmonary Disease: A Practical Guide for Clinicians. Archives of Physical Medicine and Rehabilitation, 91(1466-1470).
Duruturk, N., Acar, M., & Doğrul, M. I. (2018). Effect of Inspiratory Muscle Training in the Management of Patients With Asthma: A RANDOMIZED CONTROLLED TRIAL. Journal of Cardiopulmonary Rehabilitation and Prevention, 38(3), 198-203.
Lista-Paz, A., et al. (2023). Effect of respiratory muscle training in asthma: A systematic review and meta-analysis. Annals of Physical and Rehabilitation Medicine, 66(3), 101691.
Hoffman, M. (2021). Inspiratory muscle training in interstitial lung disease: a systematic scoping review. Jornal Brasileiro de Pneumologia, 47(4), e20210089.
Marcellis, R. G., Lenssen, A. F., de Vries, J., & Drent, M. (2013). Reduced muscle strength, exercise intolerance and disabling symptoms in sarcoidosis. Current Opinion in Pulmonary Medicine, 19(5), 524-530.
Bissett, B., Leditschke, I. A., Neeman, T., Boots, R., & Paratz, J. (2015). Weaned but weary: one third of adult intensive care patients mechanically ventilated for 7 days or more have impaired inspiratory muscle endurance after successful weaning. Heart & Lung, 44(1), 15-20.
Zaki, S., et al. (2022). Does inspiratory muscle training provide additional benefits during pulmonary rehabilitation in people with interstitial lung disease? A randomized control trial. *Physiotherapy Theory and Practice.
Bissett, B., et al. (2020). Respiratory Muscle Rehabilitation in Patients with Prolonged Mechanical Ventilation: A Targeted Approach. Critical Care, 24(103).
Bissett, B., et al. (2019). Inspiratory muscle training for intensive care patients: A multidisciplinary practical guide
Select references are listed here (frequently quoted). A complete reference list is provided in the course handout.
Menzes, K. K. P., Nascimento, L. R., Avelino, P. R., Polese, J. C., & Salmela, L. F. T. (2018). A Review on Respiratory Muscle Training Devices. Journal of Pulmonary & Respiratory Medicine, 8(451).
Gosselink, R., Troosters, T., & Decramer, M. (1996). Peripheral muscle weakness contributes to exercise limitation in COPD. American Journal of Respiratory and Critical Care Medicine, 153(976-980).
Vorona, S., et al. (2018). Inspiratory Muscle Rehabilitation in Critically Ill Adults: A Systematic Review and Meta-Analysis. Annals of the American Thoracic Society, 15(6), 735-744.
Karanfil, E. O. T., & Moller, A. M. (2018). Preoperative inspiratory muscle training prevents pulmonary complications after cardiac surgery – a systematic review. Danish Medical Journal, 65(3), A5450.
Menezes, K. K. P., et al. (2016). Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. Journal of Physiotherapy, 62(3), 138–144.
Human, A., & Morrow, B. M. (2021). Inspiratory muscle training in children and adolescents living with neuromuscular diseases: A pre-experimental study. South African Journal of Physiotherapy, 77(1), a1577.
Craighead, D., et al. (2021). Time-Efficient Inspiratory Muscle Strength Training Lowers Blood Pressure and Improves Endothelial Function, NO Bioavailability, and Oxidative Stress in Midlife/Older Adults with Above-Normal Blood Pressure. *Journal of the American Heart Association, 10.1161/JAHA.121.020980.
Janssens, L., McConnell, A. K., Pijnenburg, M., Claeys, K., Goossens, N., Lysens, R., Troosters, T., & Brumagne, S. (2015). Inspiratory muscle training affects proprioceptive use and low back pain. Medicine and Science in Sports and Exercise, 47(1), 12–19.
Severin, R., et al. (2019). Obesity and Respiratory Skeletal Muscles. In S. Walrand (Ed.), Nutrition and Skeletal Muscle (pp. 197-215). Academic Press.
Severin, R., Phillips, S. (2021). Respiratory muscle fatigability is higher in obese individuals with poor sleep quality. ERJ Open Research, 7(6). DOI: 10.1183/23120541.sleepandbreathing-2021.6.
Severin, R. S., Alshammari, S., Sherman, S. R., & Phillips, S. A. (2022). Acute Respiratory Muscle Fatigue in Patients with Obesity Following Peak Aerobic Exercise. The FASEB Journal, 36.
Caicedo-Trujillo, S., et al. (2023). Inspiratory muscle training in patients with obesity: a systematic review and meta-analysis. Frontiers in Medicine, 10, 1284689.
Ramsook, A. H., Molgat-Seon, Y., Schaeffer, M. R., Wilkie, S. S., Camp, P. G., Reid, W. D., Romer, L. M., & Guenette, J. A. (2016). Effects of inspiratory muscle training on respiratory muscle electromyography and dyspnea during exercise in healthy men. Journal of Applied Physiology, 122(5), 1267–1275.
Van Hollebeke, M., Gosselink, R., & Langer, D. (2020). Training Specificity of Inspiratory Muscle Training Methods: A Randomized Trial. Frontiers in Physiology, 11, 576595.
Ren, J. S., et al. (2022). Time to move beyond a "one-size fits all" approach to inspiratory muscle training. Frontiers in Physiology, 12.
Citation
DeMars, J. (2024). Inspiratory Muscle Training: A Review of the Evidence. Continued.com - Respiratory Therapy, Article 213. Available at www.continued.com/respiratory-therapy
