Editor’s note: This text-based course is an edited transcript of the webinar, Subacute Care Discharge Planning for the Respiratory Patient, presented by Vrati Doshi, MSc, RRT.
It is recommended that you download the course handout to supplement this text format.
Learning Outcomes
After this course, participants will be able to:
- Describe the characteristics of respiratory patients who require subacute care.
- Describe effective steps for respiratory therapists and their patients in the transition home or to subacute care.
- Explain examples of researched backed discharge plans.
With this demographic shift, health service needs will grow. Older adults often have multiple chronic conditions requiring treatment. Improved healthcare means more survivors of once terminal illnesses now require long-term care. Caring for these complex patients long-term can strain healthcare workers, including respiratory therapists.
Patient Journey
The patient's journey often continues after hospital discharge. Patients may be sent to a skilled nursing facility or receive home health care depending on their needs and current health status. Skilled nursing facilities provide 24/7 rehabilitative care and medical services for patients not yet ready to go home. The goal is to help patients regain mobility, self-care abilities, and baseline functioning so they can eventually transition home with support in place. Skilled nursing facility care plans focus on intensive rehab and nursing to improve the patient's condition.
Home health provides care to medically stable patients in their residences. Home health services include assistance with daily activities like walking, bathing, dressing, meal preparation, medication management, and overall disease management. Care plans ensure patients receive the appropriate level of care to heal and manage health conditions at home, with the coordination of intermittent skilled nursing, therapy, and aide services.
Initial Patient Destinations Following an Inpatient Hospital Stay 2020
Over half of hospital discharges return home, but many require post-acute care services to aid in their continued recovery. Post-acute care settings include skilled nursing facilities for those needing rehabilitative care and nursing services, home health for those more independent but still needing intermittent care, long-term acute care hospitals for those with complex medical needs, and inpatient rehabilitation facilities for intensive therapy.
Utilization of post-acute care services is expected to rise significantly as the population ages. By 2030, all baby boomers will be over 65, leading to a 73% increase in the number of seniors. For the first time in history, the number of people over 65 will outnumber children under 5 globally. This dramatic demographic shift will drive more older adults with chronic conditions and functional impairments to require care in skilled nursing and home health settings. Healthcare systems must prepare for escalating demand for post-acute care services.
An Aging Population and Workforce
This growing aging population highlights another challenge - 92,000 respiratory therapists, key providers of post-acute respiratory care, will retire by 2030. This impending wave of retirements coincides with escalating demands for respiratory services. Healthcare systems must prepare for this staffing cliff. Consumer preferences shaped by COVID-19 are also fueling home health growth into 2022. Value-based care has motivated providers to control costs through new methods focused on care quality over quantity. This payment model has expanded into home health and skilled nursing facilities.
Consumer Preferences and the COVID-19 Pandemic Are Key Drivers of Home Health Growth In 2022
The COVID-19 pandemic also accelerated consumer interest in at-home care. The number of home care patients increased from 5 million to 12 million by the end of 2020 as patients sought to avoid virus exposure in facilities. This surge in demand for in-home services is spearheading an expansion and transformation of home healthcare.
The growth in demand for home health is reflected in increased funding and utilization. Home health funding from Medicare and private insurance grew 9.5% from 2019 to 2020. There is also a clear aging population preference for care at home. Nearly $265 billion worth of care services, representing 25.5% of total costs for Medicare and Medicare Advantage beneficiaries, could shift from traditional facilities to home-based care by 2025 without reducing quality or access.
The COVID-19 pandemic spotlighted the vital role home health can play in alleviating strain on overburdened healthcare facilities struggling with surges in hospitalizations. Keeping vulnerable seniors and chronic disease patients healthy at home helps avoid unnecessary healthcare system utilization. Most patients agree that in-home recovery is more convenient comfortable, and reduces infection exposure risks.
Home health allows patients to continue therapy treatments started in the hospital from the comfort of home. Common home health therapies include respiratory, physical, occupational, speech and nutritional therapies tailored to manage disease and improve quality of life.
Common home health therapies include physical therapy to improve mobility and function, speech-language pathology to work on communication and swallowing disorders, occupational therapy to increase the ability to perform activities of daily living, and respiratory therapy to manage chronic pulmonary diseases and optimize breathing.
The cost savings of home-based care are significant, too. One study found substituting home care for hospital admissions reduces costs by 30% per admission while achieving equivalent health outcomes. There are many factors fueling growth in home health demand, but a key driver is simply that people want to heal and manage care in the comfort of their homes rather than facilities. The patient preference for in-home recovery and care is increasingly being heard and supported across the healthcare system.
Medicare’s Hospital Readmissions Reduction Program (HRRP)
A major value-based purchasing program is Medicare's Hospital Readmissions Reduction Program (HRRP). Since the HRRP began in 2012, hospitals have lost billions in Medicare reimbursement dollars due to readmission penalties. This drives hospitals to prioritize reducing readmissions. This penalizes hospitals for excess readmissions to encourage better care coordination and transition planning during discharge. The HRRP accelerated coordination between hospitals and post-acute facilities to align on care transition processes. Setting up communication pathways and protocols for sharing patient information is key.
Specifically, CMS looks at three prior years of unplanned hospital readmissions within 30 days of discharge, regardless of the reason for that return admission. For example, if a COPD patient is initially admitted for an exacerbation and then comes back 30 days later with pneumonia, the discharging and admitting hospital are both penalized for that readmission. The HRRP has driven more strategic targeting of patients at high readmission risk for care management. Hospitals are investing in dedicated care transition staff and post-discharge services.
The goal is to motivate hospitals to partner more closely with post-acute care providers like home health and skilled nursing facilities to ensure continuity of care after discharge. The HRRP led to the development and adoption of new quality measures around care transitions and post-acute care coordination on top of readmission rates. This allows for more robust measurement. The cumulative impact is that the HRRP is catalyzing hospitals to think beyond their four walls to build bridges with partners like home health and skilled nursing facilities. Managing patients across settings is imperative to avoid penalties and reduce costs.
This program adds further impetus for health systems to invest in smooth care transitions and the ability to manage complex patients at home to avoid readmission penalties. Adequate discharge planning is necessary to ensure patients leave the hospital with proper education on disease self-management and avoid payment reductions.
Common Respiratory Diagnosis Related Groups (MS-DRGs)
Of the top 20 most common diagnosis-related groups (MS-DRGs) discharged from hospital to homecare, four are respiratory, and for the most common readmit diagnoses, 3 are pulmonary conditions. Respiratory conditions are major drivers of 30-day hospital readmissions. Analysis shows three pulmonary diagnoses—simple pneumonia, pulmonary edema, respiratory failure, and respiratory infections and inflammations—are among the top 20 reasons for early unplanned return visits. Further, COPD flare-ups also contribute significantly to readmission rates.
Of particular concern, pulmonary edema and respiratory failure account for over 22% of all-cause 30-day readmits, while respiratory infections and inflammations with major complications or comorbidity make up another 15%. Comparatively, simple pneumonia and pleurisy with major complications or comorbidity drive roughly 19%. Still, pulmonary edema with hypoxemic respiratory failure follows closely behind.
This readmission prevalence indicates respiratory therapists have pivotal opportunities to reduce recurrence through acute and post-discharge intervention. Inpatient treatment optimization, patient and family education, discharge protocol enhancements, and transitional support coordination can better equip high-risk patients to sustain lung health outpatient.
Goal-directed respiratory therapy across the care continuum can target at-risk populations with multiple touchpoints - addressing both acute incidents and long-term disease self-management. Developing this discharge-to-home bridge is crucial for mitigating avoidable readmissions related to preventable pulmonary complications.
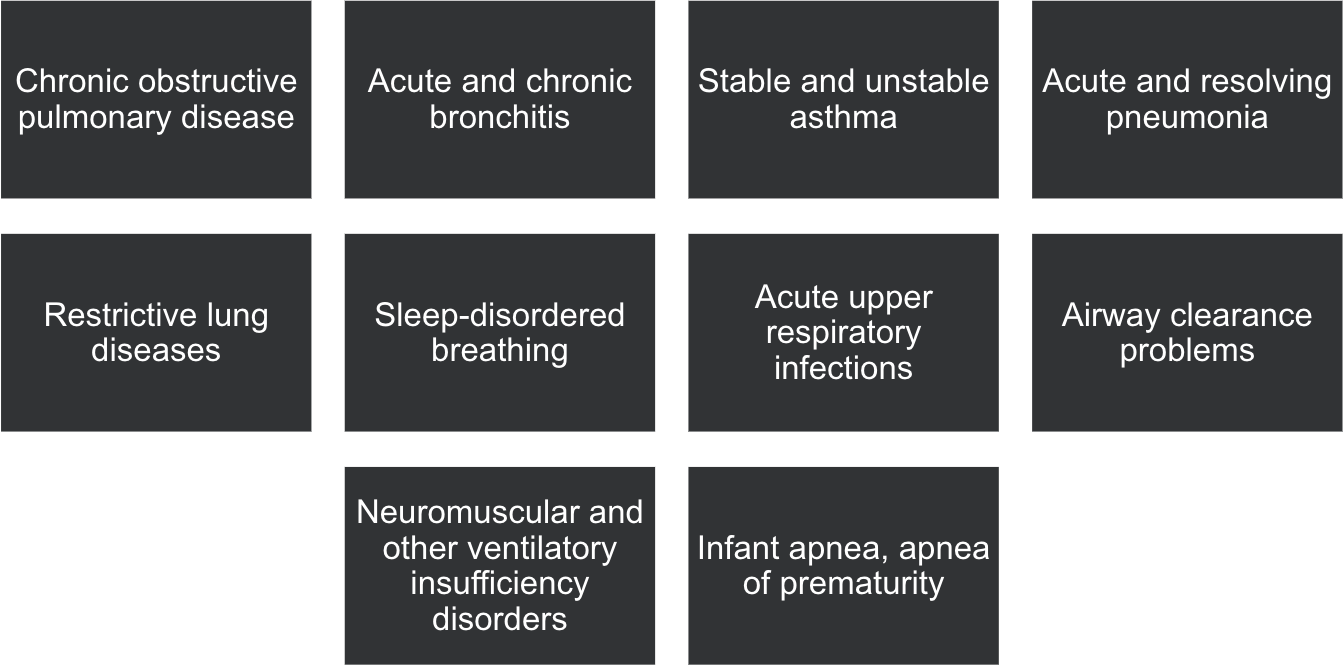
Top Respiratory Home Health Disorders
Figure 1. Top respiratory home health disorders.
In Figure 1, chronic obstructive pulmonary disease (COPD) represents a predominant respiratory disease fueling the growing utilization of home health services post-hospitalization. However, acute conditions like pneumonia, pulmonary edema, and respiratory failure following ICU stays also drive considerable skilled nursing and at-home respiratory therapy needs.
These preventable diagnoses signal opportunities to refine transitional care coordination and discharge education for at-risk groups. Patients hospitalized for pneumonia, volume overload, and hypoxemia often face a high probability of readmission within 30 days after index stay discharge. Enhancing outpatient treatment readiness for those diagnosed with recurrent lung disease can sustain capacity longer term outside the hospital.
Respiratory therapists have pivotal roles in managing both acute incidents and long-term pulmonary disease through optimized ventilation protocols, disease education, smoking cessation, airway clearance techniques, and medication/oxygen adherence coaching. Tightening gaps between inpatient and home care settings can reduce the likelihood of ER returns.
Goal-focused respiratory therapy across the entire care continuum represents a crucial link for mitigating the severity of subsequent exacerbations. As more services shift home-based, therapists must split time between bedside, transitional, and home health responsibilities to maintain incremental patient progress.
Home Respiratory Equipment
A vast array of equipment accompanies patients discharged to home care - ventilators, BiPAP, CPAP, cough assists, oxygen systems, and vest therapy. While introduced in the hospital, the transition to daily self-management proves extremely difficult. Mastering new devices alongside new diseases, medications, and an unfamiliar caregiver role is understandably overwhelming without adequate preparation and support.
Consider our own rigorous RT equipment training - part clinical engineer, part plumber. Now imagine facing that intensity as a wholly new user with a critical illness and minimal medical background. The mountain of operational, maintenance, and troubleshooting education fuels considerable anxiety, improper use, and non-adherence post-discharge.
As frontline therapists, we bear great responsibility for simplifying this transition process. Standardizing discharge coordination and hands-on training can profoundly shape patient trajectories. Thoughtful education and competency checks before discharge may provide the only chance to prepare patients functionally, mentally, and emotionally for integrating respiratory technology successfully into daily living. Our role in promoting self-efficacy persists well beyond hospital walls. The learning curve is steep, and we can play a big role in standardizing and simplifying the process of transitioning home.
When Building a Discharge Plan, Have These Outcomes In Mind
- Patient understands their condition, medications, equipment, and where to go for escalation of care
- Patient can live as independently as possible and has control over their life
- Patient can manage care at home to prevent future hospitalizations
When formulating a discharge plan, it is crucial to envision specific outcomes. Firstly, ensure that the patient comprehends their condition, medications, equipment, and knows where to seek escalated care. Secondly, empower the patient to live as autonomously as possible, asserting control over their life. Lastly, equip the patient with the ability to manage their care at home effectively, minimizing the risk of future hospitalization.
During the transition phase, whether at home or a facility, respiratory therapists play a pivotal role by undertaking significant steps to support and guide the patient. One essential aspect involves providing education about what to anticipate upon returning home or entering a skilled nursing facility. This education encompasses information about their disease state, the operation of equipment, medication management, and the appropriate contacts for escalating care. This proactive approach sets the foundation for a smoother transition and empowers the patient with the knowledge necessary for self-care.
Transition to Home or Facility
- Education on what to expect
- Disease
- Equipment
- Medication
- Who to call for escalation of care
- Include family members / caregivers
- Discuss any particulars with discharge nurse
- Patient’s ability to understand instruction
- Socio-economic implications that can impact quality of care at home
When crafting a discharge plan, keep these outcomes at the forefront. Firstly, ensure the patient comprehends their condition, medications, and equipment and knows where to seek escalated care. Secondly, empower them to live as independently as possible, retaining control over their life. Lastly, equip the patient to manage their care at home effectively, minimizing the risk of future hospitalization. The transition, whether to home or a facility, involves significant steps that respiratory therapists can take to support the patient.
Include family members and caregivers in the process. If meeting them before discharge, involve them in the conversation. Discuss specific details with a discharge nurse, such as the patient's ability to understand instructions, potential memory issues, and socio-economic factors impacting home care quality.
Consider adapting communication to the patient's level, avoiding complex language. For instance, explain tasks using relatable examples like blowing out candles. Establish a goal, whether attending a family event or celebrating a new addition, to foster a commitment to the discharge plan. Provide tools tailored to their learning style. For visual learners, create videos demonstrating equipment assembly or inhaler use. Engaging patients in this way enhances commitment to home care.
Recognize the importance of patients sharing personal information, such as job loss or home issues. This data is crucial during the handoff between departments or from hospital to post-acute care. Informing RTs and nurses about these circumstances allows them to tailor care accordingly. For instance, if a caregiver has lost their job, this information can guide the provision of assistance and education to another person in the home, ensuring continuity of care beyond the RT's presence.
Case Study
Let's delve into a compelling case study that underscores the pivotal role of a Respiratory Therapist (RT) in ensuring comprehensive care for a patient both at home and in the hospital. A 68-year-old female was discharged home with a new COPD diagnosis, accompanied by a prescription for oxygen, salmeterol, and albuterol. The durable medical equipment (DME) provider received a thorough handoff from the hospital RT, outlining the patient's history during the hospital stay. Unbeknownst to the physician, the patient, recently widowed, was now living alone. The RT proactively communicated with the primary care physician (PCP) before the initial visit, shedding light on the patient's situation.
During the in-person assessment, followed by a virtual wellness visit 72 hours later, the RT uncovered concerning issues. The patient exhibited wheezing and demonstrated incorrect medication techniques. Furthermore, the living conditions were suboptimal, with the patient appearing disheveled surrounded by dishes in the sink. Recognizing the urgency, the RT took the initiative, ordering an Uber to ensure the patient attended a sick appointment with the physician. This intervention was crucial, as the physician was unaware of the patient's post-discharge struggles. The RT's dedication went beyond the norm, conducting a virtual wellness visit to monitor the patient's progress. These findings were promptly shared with the PCP, initiating a wellness check.
- Impact of RT intervention:
- Prevention of potential COPD exacerbation and hospital readmission
- Patient admitted to SNF
- Coordinated care led to a hospital partnership between the hospital, PCP, and DME to manage respiratory patients
The collective efforts proved instrumental in averting a COPD exacerbation and potential hospital readmission. The patient, unable to manage care independently, was admitted to a Skilled Nursing Facility (SNF) instead of staying home. The coordinated care approach forged a hospital partnership involving the hospital, PCP, and DME to manage respiratory patients effectively. In summary, the proactive measures taken by the RT prevented readmission, facilitated appropriate care, and established a collaborative healthcare framework benefiting all parties involved, particularly the patient. This case exemplifies the significant impact an RT can have in ensuring holistic patient care.
Project Re-Engineered Discharge (RED)
Let's delve into the details of the discharge plan project developed by Boston University Medical Center, a culmination of seven years of work supported by funding from the Agency for Healthcare Research and Quality (AHRQ) and the National Heart, Lung, and Blood Institute. The project's primary objective was to enhance the discharge process by developing and testing activities and materials. Subsequently, they expanded the toolkit for hospital implementation. The overarching goal was to promote patient safety and contribute to a reduction in rehospitalization rates.
Crucially, the AHRQ played a pivotal role in funding the discharge toolkit for hospital implementation. This funding underscores the recognition of the project's significance in improving the quality of patient care during the crucial transition from hospital to home or another care setting. By investing seven years in research and development, the Boston University Medical Center has contributed valuable tools and strategies to healthcare institutions, aiming to optimize the discharge process and ultimately enhance patient outcomes. The collaborative support from AHRQ and the National Heart, Lung, and Blood Institute highlights the commitment to advancing healthcare practices and addressing the challenges associated with post-discharge care.
RED Components
The RED (Re-Engineered Discharge) framework encompasses a set of 12 mutually reinforcing actions, with certain actions standing out as having a direct impact on respiratory therapists. Let's explore these actions and the potential involvement of RTs in ensuring a smooth and effective transition at discharge:
- Ascertain the need for and obtain language assistance:
- RTs can play a crucial role in ensuring that patients with limited English proficiency have access to language assistance. This includes arranging for interpreters during the hospital stay and communicating this need for continued language support post-discharge.
- Make appointments for follow-up care:
- While RTs may not directly schedule appointments, they can emphasize the importance of follow-up care to both patients and their families during their interactions. Advocating for post-discharge medical appointments ensures continuity of care.
- Plan for follow-up of results from tests and labs:
- Collaborating with the care team, RTs can contribute by highlighting the importance of timely follow-up on pending test and lab results. This involves communication with the discharge coordinator to address any necessary adjustments to the patient's care plan.
- Organize post-discharge outpatient services and medical equipment:
- RTs can actively participate in coordinating outpatient services and ensuring the provision of necessary medical equipment. This involves working closely with the discharge coordinator to align hospital equipment with what the patient will use at home, reinforcing consistent education.
- Identify the correct medicines and plan for the patient to obtain them:
- RTs can reinforce medication education, especially in the case of respiratory medications. Ensuring that patients are proficient in using inhalers and understanding the prescription details contributes to a well-informed discharge plan.
- Reconcile the discharge plan with national guidelines:
- Although not solely an RT responsibility, ensuring alignment with national guidelines is crucial. RTs can collaborate with the broader care team to confirm that the discharge plan adheres to relevant guidelines.
- Teach a written discharge plan the patient can understand:
- Recognizing diverse learning needs, RTs can support patients by providing written discharge plans that cater to individual understanding. This might involve written instructions, visual aids, or notes to enhance comprehension.
- Educate the patient about their diagnosis and medications:
- From the initial encounter, RTs can consistently educate patients about their respiratory condition, emphasizing the manageable nature of diseases like COPD. This ongoing education is vital for patient empowerment.
- Review with the patient what to do when a problem arises:
- RTs can contribute by providing patients with clear action plans for potential issues. This includes educating them on whom to contact in case of emergencies or worsening symptoms, helping prevent unnecessary emergency room visits.
- Assess the degree of the patient's understanding of the discharge plan:
- RTs should actively engage patients in discussions to assess their understanding of the discharge plan. Encouraging questions and seeking feedback ensures comprehension and compliance.
- Expedite transmission of the discharge summary:
- While direct involvement in transmission may not be an RT responsibility, collaboration with the care team ensures that key information is conveyed during the handoff to clinicians providing post-discharge care.
- Provide telephone reinforcement of the discharge plan:
- RTs can contribute to reinforcing the discharge plan through telephone follow-ups. This involves checking in with patients, answering questions, and addressing any concerns, promoting continuity of care beyond the hospital.
In summary, RTs can actively participate in several key actions outlined in the RED framework, contributing to the overall success of patient transitions and reducing the likelihood of readmission. Their involvement is particularly impactful in actions that directly relate to respiratory care and patient education.
RED Hospital Implementation
- How to begin implementation at your hospital
- How to deliver the Re-Engineered Discharge
- How to deliver the RED to diverse populations
- How to conduct post-discharge follow-up telephone call
- How to monitor RED implementation and outcomes
The RED toolkit offers comprehensive guidance for hospital implementation, covering essential steps to enhance the discharge process. Let's delve into the key components outlined in the toolkit:
- How to Begin:
- The toolkit is initiated by exploring the advantages and disadvantages of integrating discharge education functions into the responsibilities of the staff nurse responsible for patient discharge. It also considers the option of hiring dedicated discharge educators for these functions. This step is crucial for determining the most effective strategy for implementing the RED components within the hospital setting.
- Tasks for Discharge Educators:
- This section outlines various tasks that discharge educators can undertake to implement RED components. Tasks range from reconciling medicine lists to reviewing the After Hospital Care Plan (AHCP) with the patient. The toolkit provides instructions on creating an AHCP—a patient-friendly booklet with clear instructions on self-care after hospital discharge.
- Delivering the RED to Patients from Diverse Backgrounds:
- Recognizing the diversity among patients, this step focuses on delivering RED to individuals from varied backgrounds, including considerations for language, culture, race, ethnicity, education, literacy, and social circumstances. Ensuring that discharge education is accessible and tailored to diverse needs is crucial for effective implementation.
- Post-Discharge Reinforcement and Phone Call:
- A critical component this step involves scheduling a phone call within 72 hours of a patient's hospital discharge. The objectives include reviewing appointments, medicines, addressing medical issues, and providing guidance for non-emergent problems. The toolkit offers a script for the phone call, a documentation form, and a role-play script for training callers, ensuring consistency in post-discharge follow-up.
- Examine Readmission Rates and Implement Monitoring Programs:
- To drive continuous improvement, the toolkit encourages hospitals to examine current readmission rates and implement monitoring programs. It emphasizes the reasons for measuring transitional care, suggests implementation and outcome measures, and reviews the availability of data to create benchmarks. This step is essential for hospitals to assess their progress and make informed adjustments.
In summary, the RED toolkit provides a structured approach for hospitals to enhance the discharge process. From initial considerations of how to begin to the detailed tasks discharge educators should undertake, the toolkit addresses the multifaceted aspects of patient transition from hospital to home. The emphasis on diverse patient backgrounds, post-discharge reinforcement, and ongoing monitoring ensures a comprehensive and patient-centered approach to transitional care.
Impact of RED
The impact of the RED (Re-Engineered Discharge) framework is substantial, as evidenced by the following key findings:
- 30-Day Readmission Decrease:
- Implementation of the RED framework resulted in a remarkable 25% decrease in 30-day readmissions. This reduction is a significant indicator of the effectiveness of the discharge process improvements facilitated by RED.
- Cost Savings per Patient:
- The implementation of RED led to a cost savings of $412 per patient. This financial impact is a testament to the efficiency and positive outcomes associated with the RED framework.
- Prevention of Readmissions or ED Visits:
- Notably, one readmission or Emergency Department (ED) visit was prevented for every seven patients who received RED. This statistic underscores the preventive nature of the RED framework, contributing to improved patient outcomes and healthcare resource utilization.
- Lower Observed Cost:
- RED demonstrated a lower observed cost of 33.9%, emphasizing the potential for significant cost savings in healthcare delivery. This reduction in cost aligns with the broader goal of optimizing resource utilization and improving the overall efficiency of care.
- Improved Primary Care Follow-Up:
- The RED framework facilitated improved primary care follow-up, a critical aspect of post-discharge care. A nurse discharge advocate actively worked with patients during their hospital stay, arranging follow-up appointments, ensuring medication reconciliation, and conducting patient education. This personalized approach contributed to better patient engagement and adherence to the discharge plan.
The study utilized a randomized trial design involving English-speaking hospitalized adults with a mean age of approximately 50 years. The trial was conducted in general medical service at an urban academic safety net hospital, involving 749 participants. Funding from reputable organizations, including the Agency for Healthcare Research and Quality, the National Heart and Lung and Blood Institute, and the National Institute of Health, underscored the significance of the research.
Given the success of the RED framework, particularly in the roles played by discharge nurses and pharmacists, there is potential for respiratory therapists (RTs) to adopt similar responsibilities in follow-up care. RTs could actively engage in post-discharge calls, reinforcing education, ensuring equipment adherence, and contributing to the reduction of costs and readmissions. This approach aligns with the patient-centered and comprehensive care principles promoted by the RED framework. It provides an opportunity for RTs to play a vital role in enhancing the continuity of care for patients transitioning from the hospital to home.
COPD Caregiver’s Toolkit
The COPD Caregivers Toolkit, launched by the Respiratory Health Association (RHA) with support from the National Heart Lung and Blood Institute's Learn More, Breathe Better Program, has proven to be highly effective. In a study conducted in 2018 to assess the toolkit's acceptance, notable findings were observed:
- High Acceptance Rate:
- The study revealed that 68% of participants found the COPD Caregivers Toolkit helpful. This high acceptance rate indicates that the toolkit effectively addresses the needs of caregivers in supporting individuals with COPD.
- Recommendation Rate:
- An impressive 92% of participants stated that they would recommend the toolkit to someone else. This strong endorsement underscores the perceived value and utility of the toolkit among caregivers.
Designed with a focus on supporting caregivers rather than the patients themselves, the COPD Caregivers Toolkit serves as a valuable resource for those involved in the care of individuals with COPD. This includes respiratory therapists (RTs) working on the home side or in skilled nursing facilities who can provide the toolkit to patients' families during the discharge process. The toolkit offers comprehensive support by providing caregivers with essential information on who to contact, what to expect, and an educational component on the COPD disease state. This proactive approach ensures that caregivers are well-equipped to manage the care of COPD patients effectively, contributing to better patient outcomes and overall caregiver satisfaction.
For RTs, incorporating the COPD Caregivers Toolkit into the discharge process can enhance the continuum of care by extending support beyond the patient to their caregivers. By empowering caregivers with the necessary resources and information, RTs contribute to a more informed and capable support system for individuals managing COPD in a home or skilled nursing facility setting. The COPD Caregivers Toolkit, structured around five common questions, is designed to provide practical and accessible support for caregivers. The toolkit addresses key areas of concern for individuals caring for someone with COPD, making the information easily understandable through a combination of visuals and text. The simplicity of the content ensures that it can be comprehended by individuals up to a fifth-grade level. Let's explore the questions and topics covered in the toolkit:
- How do I help the person I'm caring for manage COPD?
- This section likely includes guidance on assisting with medication management, recognizing symptoms, and supporting the individual in adopting a healthy lifestyle to manage COPD effectively.
- What should I know about managing at home for someone living with COPD?
- This may cover aspects such as creating a COPD-friendly living environment, understanding the use of respiratory equipment, and ensuring a safe and comfortable home setting.
- How do I prepare for a visit to the doctor?
- Caregivers can benefit from information on preparing for medical appointments, questions to ask healthcare providers, and understanding the importance of regular check-ups for COPD management.
- How do I help after a COPD flare-up or hospital stay?
- This section likely provides guidance on recognizing signs of a flare-up, responding to emergencies, and supporting the individual's recovery following a hospital stay.
- How do I take care of myself while managing someone else's care?
- Caregiver self-care is crucial, and this section may include tips on managing stress, seeking support, and ensuring that caregivers prioritize their own well-being.
The toolkit's emphasis on simplicity and visual elements enhances its accessibility, ensuring that caregivers of varying literacy levels can effectively utilize the information. By structuring the toolkit around these common questions, it provides a practical and user-friendly resource for caregivers navigating the challenges of supporting someone with COPD. This approach aligns with the goal of empowering caregivers with the knowledge and tools they need to provide effective care at home.
Research on Discharge Plan Effectiveness
- Systematic review focused on effects of early follow-up after hospital discharge for patients with heart failure or COPD
- Randomized controlled trail, 2 non-randomized controlled trials, and 7 observational studies
- Early follow-up was associated with reduced risk of all-cause readmission, ED visits, and mortality
A 2021 systematic review and meta-analysis examined the impact of early outpatient follow-up after discharge for patients hospitalized with heart failure or chronic obstructive pulmonary disease (COPD). The analysis pooled data from 10 studies - 1 randomized controlled trial, two non-randomized controlled studies, and seven observational cohort studies. In total, the review included 24,730 patients admitted with decompensated heart failure or acute exacerbation of COPD.
Across all studies, an early follow-up visit within 7-30 days of hospital discharge was associated with significantly reduced risks of all-cause hospital readmission, emergency department revisits, and all-cause mortality compared to routine follow-up. Specifically, early clinician follow-up decreased relative odds of readmission by 11%, ED visits by 20%, and mortality by 17%. These findings remained consistent even in sensitivity analysis of the highest quality studies.
Notably, one RCT found a clinic visit within one week of discharge effectively reduced 90-day readmission for high-risk heart failure patients by 36%. The systematic review concluded that early outpatient follow-up represents an impactful, low-cost intervention to improve outcomes after heart failure or COPD hospitalization.
- Randomized clinical trial studied outcomes of standardized transition bundle and care coordinator for patients with acute exacerbations of COPD
- Transition bundle cohort were 83% less likely to be readmitted within 7 days and 26% less likely to be readmitted within 30 days of discharge
- Care coordinator did not influence readmission or ED revisits
A 2022 randomized clinical trial examined the impact of implementing a standardized care transition bundle, with or without an assigned care coordinator, for patients hospitalized for acute exacerbation of COPD. The transitional bundle included enhanced education on disease self-management, medication reconciliation, as-needed action plans, follow-up scheduling, and post-discharge needs assessment. The study randomized 568 COPD patients from 2 hospitals to receive either:
- Usual care
- Transition bundle
- Transition bundle plus assigned care coordinator
The main outcome measures were 7-day and 30-day all-cause and COPD-related readmission rates, as well as ED revisits. The transition bundle group demonstrated significantly lower 7-day readmission - 83% relative risk reduction compared to usual care. The bundle also reduced 30-day readmits by 26%. However, adding a dedicated care coordinator did not confer any additional reduction in readmissions or ED visits. The findings highlight the potential for standardized transition protocols to dramatically improve short-term outcomes for COPD without increasing resource use. Implementation would require interdisciplinary coordination with respiratory therapy to identify high-risk patients pre-discharge.
The insights from these studies highlight the importance of early follow-up and the potential benefits of standardized transition bundles with care coordination. However, it's noteworthy that there is a lack of large, methodologically robust studies specifically focused on the effectiveness of discharge plans for respiratory patients. While there are studies on COPD protocols, much of the emphasis is on nursing care and discharge planners in education and follow-up.
The potential influence of clinicians over care coordinators in readmission outcomes suggests that the roles of different healthcare professionals in the discharge process may have varying impacts. Additionally, replicating some of these studies with a focus on respiratory therapists and their effects on patient care at home and during the discharge process is valuable. This could contribute to a more comprehensive understanding of the role of respiratory therapists in improving outcomes for respiratory patients post-discharge.
In summary, the studies mentioned underscore the importance of early follow-up and the potential benefits of specific interventions in reducing readmissions. There is an opportunity for future research to delve deeper into the specific contributions of respiratory therapists in discharge planning and post-discharge care for respiratory patients.
Respiratory Therapists Taking the Extra Step
Respiratory Therapists (RTs) can collaborate with home care and DME companies to establish a clinician-to-clinician handoff document. This document includes crucial particulars about patients and their family caregivers, especially when dealing with diverse languages, the presence of babies or pets in the home, and assessing the availability of proper electricity for equipment. It is essential to ensure that patients discharged with oxygen have the necessary facilities at home to manage their care effectively. Key considerations include evaluating the patient's ability to take medications correctly and determining if they require constant reminders. Standardizing education is paramount, fostering continuity in communication and care. Utilizing toolkits that maintain consistent communication from the hospital to home reinforces crucial information.
Incorporating videotaped techniques demonstrating equipment cleaning, medication administration, and disease state explanations provides valuable resources for patients and their families to reference. Encouraging patients to document key points during education, akin to taking notes in school, enhances retention. In summary, the shift in care delivery from facilities to homes necessitates robust and standardized processes to minimize hospital readmissions. Discharged respiratory patients require comprehensive education on their diseases, medications, equipment, and self-management. RTs can significantly contribute to patient satisfaction and long-term quality care. It is recommended to consider implementing a standardized discharge protocol tailored specifically for respiratory patients.
Questions and Answers
Do you think we often miss the window of opportunity to apply long-standing solutions in our profession?
Presenter: I won't dismiss the potential inherent in these opportunities; I firmly believe that possibilities abound. Attending webinars like the one we're engaging in now offers a chance to ignite meaningful conversations. It's an avenue to observe the innovative practices shaping our field, allowing us to return to our departments armed with insights and possibilities. These forums empower us to pose the question: Can we implement similar strategies in our own setting? Consider, for instance, the COPD toolkit—a valuable and complimentary resource. Accessible through download or order from the Respiratory Health Association, this toolkit is a tangible asset that can be readily stocked in both clinical departments and on the home health side. Here lies an opportunity waiting to be seized. It involves actively participating in departmental discussions and, when needed, elevating the discourse to higher levels. Collaborating with the pulmonary department to establish it as a standard of care is an impactful role that Respiratory Therapists (RTs) can play. Engaging with nursing staff and physicians, RTs can present compelling studies and their outcomes. The pertinent question then becomes: Can we integrate these findings into our department's practices, especially for COPD patients entering the ED or ICU? It's not a matter of missing opportunities; rather, it's an ongoing pursuit of optimizing patient care to the best of our abilities. In most hospitals, a discharge planning committee is typically led by a nurse who serves as the nexus of resources available to patients upon departure. This encompasses a comprehensive array, including vendor lists for home care and durable medical equipment (DME). Collaborating with this discharge planning nurse becomes crucial for Respiratory Therapists (RTs). It involves assessing the proficiency of home care companies in respiratory care. If there's a gap in knowledge, introducing the discharge planning tool to these entities becomes an imperative step. Engaging with discharge planning nurses in this manner is not just beneficial for patient care; it also aligns with the interests of these home care companies. Those on the preferred provider list inherently desire to fulfill the hospital's expectations. By equipping them with the tools and knowledge specific to respiratory care, we create a win-win scenario. These seemingly minor interventions can make a significant impact, fostering better care for the patient. It's about being a staunch advocate for the patient's well-being and using our influence to push for elevated standards of care.
How does the dynamic nature of various components in the discharge plan, evolving from the beginning to the end of patient care, contribute to promoting patient safety?
Hospitals aim to minimize readmissions, emphasizing the importance of patient safety. Educating patients throughout the team is key, enabling them to implement these measures upon discharge and further reducing the risk of readmission. This aspect resonated with me. In terms of patient safety, hospitals have a vested interest in adopting toolkits and resources to prevent readmissions. Anything that aids in reducing costs and facilitating earlier discharges aligns with the hospital's goals. The RT department plays a crucial role in championing these initiatives, and while many are open to listening, it requires a strong voice within the RT department to effectively advocate for these practices.
Is the toolkit something that we are able to access and download?
To access the COPD toolkit, you can visit the Respiratory Health Association website and navigate to the "Resources" tab. There, you'll find the COPD toolkit available for download or bulk ordering for your facility. It's recommended to provide this toolkit to any new patient diagnosed with COPD and their caregivers present in the room. The widespread distribution of this toolkit is beneficial, as evidenced by positive outcomes data. Users have found it highly helpful, and its utilization can extend to friends and family who may also be dealing with COPD. Furthermore, the toolkit serves as an objective measuring tool. It facilitates the collection of essential information from patients, enabling effective communication with relevant team members such as physicians, nurses, and family members. This structured approach helps prevent miscommunication, ensuring that the information conveyed remains accurate and consistent throughout the healthcare team.
Can the COPD toolkit be used one time, or is it applied both initially and periodically throughout the patient's care journey?
Certainly, I would recommend providing the COPD toolkit to a patient during the initial encounter, particularly when dealing with a new COPD diagnosis. It's beneficial to walk them through the various components of the toolkit. The COPD toolkit is specifically designed for caregivers, allowing you to give it to both the patient and their caregiver. This approach reinforces the support structure that the patient will have at home. For individuals managing COPD at home, the multitude of educational pamphlets provided during hospital visits—accompanying new diagnoses or medications—can be overwhelming. The toolkit serves as a simplified resource, helping caregivers organize and comprehend the information effectively. It streamlines expectations, such as the need for the patient to take medication multiple times a day or use specific equipment for secretion removal. Caregivers gain insights into the level of support required at home, addressing nuances like ensuring accessibility to equipment for less mobile patients. The toolkit proves crucial in highlighting these subtleties, especially for those transitioning to the home care setting. By distributing it from the outset, caregivers have the opportunity to familiarize themselves with the contents, seek clarification, and return with any questions before the patient's discharge. This ensures that key information is reiterated and thoroughly understood.
Why are the respiratory diagnoses so high in readmissions? What are we missing?
Absolutely, it is a critical question to consider. Respiratory patients often present with a multitude of comorbidities, extending beyond respiratory issues to encompass conditions like heart problems and diabetes. The aging population, largely consisting of baby boomers, includes a substantial number of smokers and ex-smokers, contributing to the prevalence of complex health challenges. With this demographic shift, a growing number of individuals are grappling with various health issues and leaving hospitals without adequate education or support for home care. The challenges intensify as the aging population faces a shortage of caregivers—a reality underscored during the COVID-19 pandemic. This shortage extends beyond hospitals to encompass home care, impacting respiratory therapists, nurses, and physicians alike. Consequently, there's an escalating demand for care while the available support for patients is diminishing. A noticeable gap emerges wherein patients receive care at the hospital, but its adequacy for discharge may vary. Upon returning home, they encounter difficulties managing their care, grappling with multiple medications, unfamiliarity with equipment usage, and the complexity of dealing with various vendors for different aspects of their care. The intricacies are compounded for patients lacking a robust support system. Even with a healthcare background, navigating insurance, finding a covered primary care physician (PCP), identifying pharmacies that deliver medications, and addressing other healthcare-related queries can be challenging. Respiratory patients, often dealing with chronic conditions, require ongoing care. The recurrent readmissions observed in these cases underscore the need for a comprehensive and continuous support system. In some instances, the ease of seeking emergency care may appear more appealing than waiting for a physician's appointment, emphasizing the chronic nature of these healthcare challenges.
How can we address the challenge of patients who may not realize the questions they need to ask during their healthcare journey, leading to a sudden influx of overwhelming queries after the acute care phase?
The RED toolkit includes a section with suggested questions to ask healthcare providers such as primary care physicians or pulmonologists. These questions cover aspects like insurance coverage, follow-up appointments, and coordination with DME and pharmacies. Patients may not be aware of these questions, and physicians might lack time to address them comprehensively during visits. In this context, respiratory therapists (RTs) play a significant role, even in reactive situations when patients are already ill upon hospital admission. Educating patients during such overwhelming moments is crucial. Recognizing the complexity of healthcare transitions, utilizing toolkits, and speaking up early can help eliminate barriers, creating a positive domino effect for patients and their families. Despite the challenges RTs may face in gaining attention, finding influential champions within the healthcare system, such as supportive physicians, nurses, or department heads, can drive change. Utilizing evidence-backed approaches and emphasizing the business aspect of healthcare can facilitate the acceptance of initiatives like implementing toolkits, especially when they are offered for free and endorsed by reputable agencies. The gradual nature of change in healthcare emphasizes the importance of building support from key stakeholders.
How can we navigate and overcome common barriers encountered, whether as an RT, nurse, or physician? Examples include dealing with patients or team members lacking enthusiasm for consistent communication, addressing tension within multidisciplinary teams, or assisting patients who don't speak English as their primary language. How do we effectively navigate these challenges?
In the realm of respiratory therapy, individual differences among practitioners are inevitable. We've all encountered environments where dedication levels vary. When you, as an RT, consistently go above and beyond, you are inherently prioritizing patient care. Continuing to uphold these standards is crucial. While disparities in enthusiasm among RTs may become apparent, especially when it affects patient outcomes, it's imperative to communicate such concerns to department heads. Advocating for standardized practices ensures that efforts to improve patient care, such as introducing new toolkits, are embraced across the entire respiratory department. Reflecting on my experience in an ICU with a service-based model, where all RTs adhered to the same protocol, it became evident that a unified approach fosters enthusiasm. Having a shared education script and learning from each other created a contagious enthusiasm. However, disparities in enthusiasm can be detrimental, impacting patient care. Initiatives should focus on creating an infectious culture where all RTs contribute to standardized practices. In a hospital situated in the culturally diverse city of Chicago, language barriers were a common challenge.
Employing strategies such as interpreter services and enlisting nurses fluent in the patient's language proved effective. Collaborating with colleagues who shared language skills not only facilitated communication but also fostered camaraderie among clinicians. Encouraging patients to bring in caregivers during hospital stays for comprehensive education, utilizing interpreter lines, and recording bilingual instructions contribute to setting patients up for success at home. Consistency in communication is vital for patient understanding. Breaking down education into manageable chunks aligns with patients' routines and enhances retention. While the timing may vary based on individual circumstances, providing information incrementally allows patients and their families to absorb, record, and ask questions. The goal is to create a supportive environment that encourages ongoing communication, ensuring that patients feel confident managing their care beyond the hospital stay. Some of the interventions that we did when we were in the hospital were because it was an academic hospital, where a substantial number of residents rounded regularly. We identified key gaps in their understanding of respiratory therapy, particularly when it came to ventilators and durable medical equipment (DME). Physicians generally possess a foundational knowledge of anatomy but may lack specific expertise in equipment and medication intricacies. Recognizing this, our respiratory department took the initiative to enhance overall understanding and communication among healthcare professionals. Acknowledging the absence of a dedicated course for physicians on ventilators and DME, we implemented a series of 15-minute courses throughout the year. These sessions aimed to reinforce effective communication with patients and ensure that both nursing teams and physicians were equipped with the necessary knowledge. The approach was well-received, emphasizing collaboration rather than condescension. We emphasized the importance of being collectively well-informed to guarantee that patients leave the hospital with a comprehensive understanding of equipment usage.
Encountering situations where patients had nebulizers running without medication due to incomplete instructions, we viewed these instances as opportunities for education rather than shortcomings. The respiratory department actively engaged nursing teams, offering assistance without judgment and encouraging future collaboration. By providing clear guidelines on equipment use and communicating openly, we successfully fostered a cohesive team dynamic. Over time, our department became recognized as experts, not only in respiratory care but across various aspects of patient management. Recognizing the importance of a unified approach, I stress the significance of showing the value of our expertise through actions. While one person cannot carry the entire team, having a strong leader who listens, pays attention, and champions evidence-based initiatives are crucial—establishing trust within the multidisciplinary team and showcasing the ability to teach and ensure patient well-being positions respiratory therapists as vital contributors in various healthcare aspects. This collaborative approach and effective communication are pivotal for achieving comprehensive and patient-centered care.
How important is networking?
Absolutely, networking is a crucial element. Demonstrating your value within the team is not only beneficial for your department and the respiratory field but also impacts the long-term trajectory of patient care. You never know the lasting effects of your contributions. Patient safety is paramount, and ensuring that the patient receives the care they need is the ultimate goal.
I work in the hospital setting, and we have an eval and treatment protocol that MDs will order as RCP. We evaluate the patient and develop a care plan for the patient while they are in the hospital. What are ways that we can help manage the care at home?
Firstly, that iss fantastic. Not all hospitals have such protocols. To manage care at home effectively, consider creating a document for the patient's chart or discharge planner. Include details about the patient's home environment, such as living alone, recent life changes, or any factors affecting care. Outline the treatment provided during the hospital stay, including educational videos, and note the patient's understanding and motivation for improvement. Highlight upcoming events or milestones important to the patient, as this can serve as a motivator for both the patient and the RT managing care at home. Foster relationships with home care organizations and ensure a smooth handoff of information between hospital and home RTs. Advocate for the patient's needs, ensuring that the receiving facility, whether home health or a skilled nursing facility, is equipped to manage respiratory patients. Leverage your relationship with the discharge coordinator to communicate crucial information for effective post-hospital care. Managing the care transition from hospital to home involves collaboration and effective communication, ensuring the patient continues to receive comprehensive and tailored respiratory care.
Is it important to have a well-defined plan and process, ensuring continuity of care and the seamless transfer of information between facilities, even if the information is documented electronically in systems like Epic or other hospital systems?
In the case of readmission, especially for frequent flyers, having a documented history proves invaluable. With prior documentation, you can recall details about the patient, such as recent widowhood, allowing you to approach them with empathy and discuss relevant aspects of their care. Inquiring about their experiences at home and any potential improvements they would suggest enables you to gather crucial insights. It becomes your responsibility to ensure that the primary care provider, nurse, and coordinator are well-informed about the factors contributing to the patient's return, facilitating better care coordination. As a hospital RT, the post-discharge phase typically involves a hands-off approach. However, establishing a system, be it in the form of documentation or communication with the coordinator, becomes crucial. These measures are important not only for advocating for the patient but also for contributing to more informed and effective care. Recognizing the significance of socioeconomic factors and identifying barriers to care is a process that may not yield immediate results but can lead to substantial positive outcomes in the long run. These seemingly minor adjustments and insights into patient motivation can have a profound impact on the patient, their family, the hospital, and your role as an RT.
References
Bestsennyy, O., Chmielewski, M., Koffel, A., & Shah, A. (2022, February 1). From facility to home: How healthcare could shift by 2025. McKinsey & Company. https://www.mckinsey.com/industries/healthcare/our-insights/from-facility-to-home-how-healthcare-could-shift-by-2025.
The COPD Caregiver’s Toolkit | NHLBI, NIH. (n.d.). NHLBI, NIH. https://www.nhlbi.nih.gov/education/copd-learn-more-breathe-better/copd-caregivers-toolkit.
Haddad LM, Annamaraju P, Toney-Butler TJ. Nursing Shortage. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
Holly, R., & Holly, R. (2021, December 15). Accelerated by pandemic relief programs, national home health spending hits $123.7 billion. Home Health Care News. https://homehealthcarenews.com/2021/12/accelerated-by-pandemic-relief-programs-national-home-health-spending-hits-123-7-billion/.
Hosp. Readmission Reduction | CMS. (n.d.). https://www.cms.gov/medicare/quality/value-based-programs/hospital-readmissions.
Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O'Donnell JK, Paasche-Orlow MK, Manasseh C, Martin S, Culpepper L. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009 Feb 3;150(3):178-87.
Le, N. C., Rahman, T., Kapralik, J. L., Ibrahim, Q., Lear, S. A., & Van Spall, H. G. C. (2022). The Hospital at Home Model vs Routine Hospitalization for Acute Heart Failure: A Survey of Patients’ Preferences. CJC Open, 4(3), 263-270.
Leaders, O. T. (2019, April 19). 4 major In-Home Healthcare Market Drivers to watch. HIT Consultant Media. https://hitconsultant.net/2019/04/18/4-major-in-home-healthcare-market-drivers-to-watch/.
McIlvennan, C. K., Eapen, Z. J., & Allen, L. A. (n.d.). Hospital Readmissions Reduction Program. Circulation. https://doi.org/10.1161/circulationaha.114.010270.
Mcconnell, T. (2022, March 3). 2022 Outlook: Home Health and Hospice - HealthCare Appraisers. HealthCare Appraisers. https://healthcareappraisers.com/2022-outlook-home-health-and-hospice/
Popowitz, E. (n.d.). The growing demand for at-home care. Definitive Healthcare. https://www.definitivehc.com/blog/growing-demand-home-care.
Project RED (Re-Engineered Discharge): Toolkit. (n.d.). https://www.bu.edu/fammed/projectred/toolkit.html.
Citation
Doshi, V (2023). Subacute care discharge planning for the respiratory patient. Continued.com - Respiratory Therapy, Article 208. Available at www.continued.com/respiratory-therapy