Editor’s note: This text-based course is an edited transcript of the webinar, A Team Approach for Sleep Apnea, presented by Dr. Kelvin Imo, DDS, IAOS-Diplomate Candidate.
Learning Outcomes
After this course, participants will be able to:
- Describe the brief history of sleep apnea
- Recognize the multidisciplinary team approach for sleep apnea
- Explain the benefits of a multidisciplinary approach for patient-centered care
- List 3 disciplines who are part of the treatment team for sleep apnea management
- Identify the important role of health care providers working together vs. separately for sleep apnea management
Introduction
We are talking about a team approach, and I would like to share what got me so involved in sleep. In 2018, I had a stroke. I saw many providers who never tested me on how I sleep. I am five foot eight, 165 pounds, maybe 170 after having a good meal, and it never came up. I am pleased and thankful for this opportunity to talk to you about sleep within a team approach.
Etymology of Team
- Where Does It Come From and What Does It Mean?
- Etymology of a team is applied in Old English to groups of persons working together for some purpose, especially “group of people acting together to bring suit.” In modern times translates to “persons associated in some joint action” (Etymonline.com)
Brief History of Sleep Apnea
Let's look briefly at the history of sleep apnea.
- 1907-Intro of sleep in non-sleepy dogs using serum, take hypnotoxin theory to its zenith
- 1920- Sleep deprivation results in greater sleepiness in the night than the following morning-beginning of understanding of circadian drive to sleep (Kleitman, 1982)
- 1928- Discovery of EEG- the end of the “Resting Brain” theory of sleep
- 1949- The discovery of the reticular formation and the role of the RAS ascending arousal system
- 1953- Discovery of rapid eye movements and REM sleep (Aserinsky & Kleitman, 1953)
- 1965- Reports of apnea like activity ignored (French and German groups)
- 1970- Italian group fully describes obstructive sleep apnea (OSA) events including the occurrence of OSA in nonobese patients and cardiovascular comorbidities.
- Dement opens first sleep clinic at Stanford
- 1975- The origins of the American Academy of Sleep Medicine
- First qualification tests for specialty 1977
- 1980- Sullivan introduces CPAP
- 1985- The first description of the need for a multidisciplinary approach
Multidisciplinary Approach Tried
- 1985- Presbyterian Hospital Sleep Disorders Center in Oklahoma City, OK tried the approach
- Involved sleep physiologist, otolaryngologist, a pulmonologist, and a neurologist
- 1996- Prince Charles Hospital, Brisbane, Australia
- Involved a thoracic physician, ENT, and dental colleagues
- 2016- Tripler Army Medical Center Multi-D Clinic, Honolulu, Hawaii-Involved an ENT, oral surgeons, sleep medicine physicians and expanded to more disciplines
Sleep apnea treatment was to be done under one umbrella in one facility. We are going to see some hang-ups or issues that this multi-disciplinary approach brings about when trying to do it under one umbrella. We will speak on how we can at least think about our role as individuals to treat OSA with a broad point of view, still with one common goal: a successfully treated OSA patient.
Why is the Multidisciplinary Approach Uncommon?
The first thing we think of, there are many challenges. The big challenge is the cost. We live in a society where it is trying to minimize costs in healthcare. The second thing, medicine appears to be going in the opposite direction. Group clinics have one provider who sees multiple patients for cost efficiency. Another thing you run into now requires buy-in from physicians from various disciplines and the healthcare administration. We have many disciplines, but before we go into the disciplines, it comes to believing.
Napoleon Hill
The great Napolean Hill said, "Whatever your mind can conceive and believe, it can achieve." In general, this applies not just in healthcare but pretty much in life in general. Whatever our minds can conceive and believe, we will achieve it.
The Fight
If we sit back and start to think about it, what are we up against? The sleep issue is going on here in the United States and throughout our world. How do we attack this belief versus believing? I like to look at it as the "fight." Not that we are in a physical fight, it is a fight of the mind to make a shift. It is a talked-about belief, and what we believe in is what we can achieve.
What Will You Do?
Let's look at the numbers:
- 50 to 70 million adults in the U.S. are affected by a sleep disorder
- 25 million adults in the U.S. have obstructive sleep apnea
- 80% of the 25 million are undiagnosed (American Sleep Association, 2021)
I want us to look at the numbers, and you have heard the saying, numbers do not lie. About 50 to 70 million adults in the United States are affected by a sleep disorder. There are roughly 258 million adults in the United States. According to the 2020 Census Bureau, 25 million adults have obstructive sleep apnea in the United States. Yes, 25 million people resonate profoundly. Out of that 25 million, 80% are undiagnosed. This means that 20 million Americans walk around with obstructive sleep apnea and do not know. Now, we come to that "fight" we believe in. You have these people, but how do we get to these people?.
Stop! Think!
- How can we achieve this?
- What role do you and I play?
- I challenge you to be a committee of ONE!
- Let's change our mindset and make this a reality
If you look at it in detail, 1 in 12 suffer from obstructive sleep apnea. We ask ourselves, what will I or you do? During the holidays, think about Thanksgiving. I assume many people will get together, maybe a group of 12 or more people. Of those 12, at least one will have sleep apnea, and is this person being treated? Have they been assessed? We have to stop and think about how can we achieve this? What role do you and I play as providers or laypeople? What do we do to reach the 12 or the 20 million undiagnosed people? If we challenge ourselves to be a committee of one, you could be the individual, like I was that person. I am a person who has sleep apnea. We have to think about how to take care of that person. Do we notice certain things they do if it is our loved ones? Are we helping them stay active? Are they going to their providers? Moreover, this involves a mindset shift. There is a saying to "think outside the box." There is a problem with thinking that there is a box already. What if we think there is "no box" and what we can do as individuals, arriving at a common goal.
Oropharynx
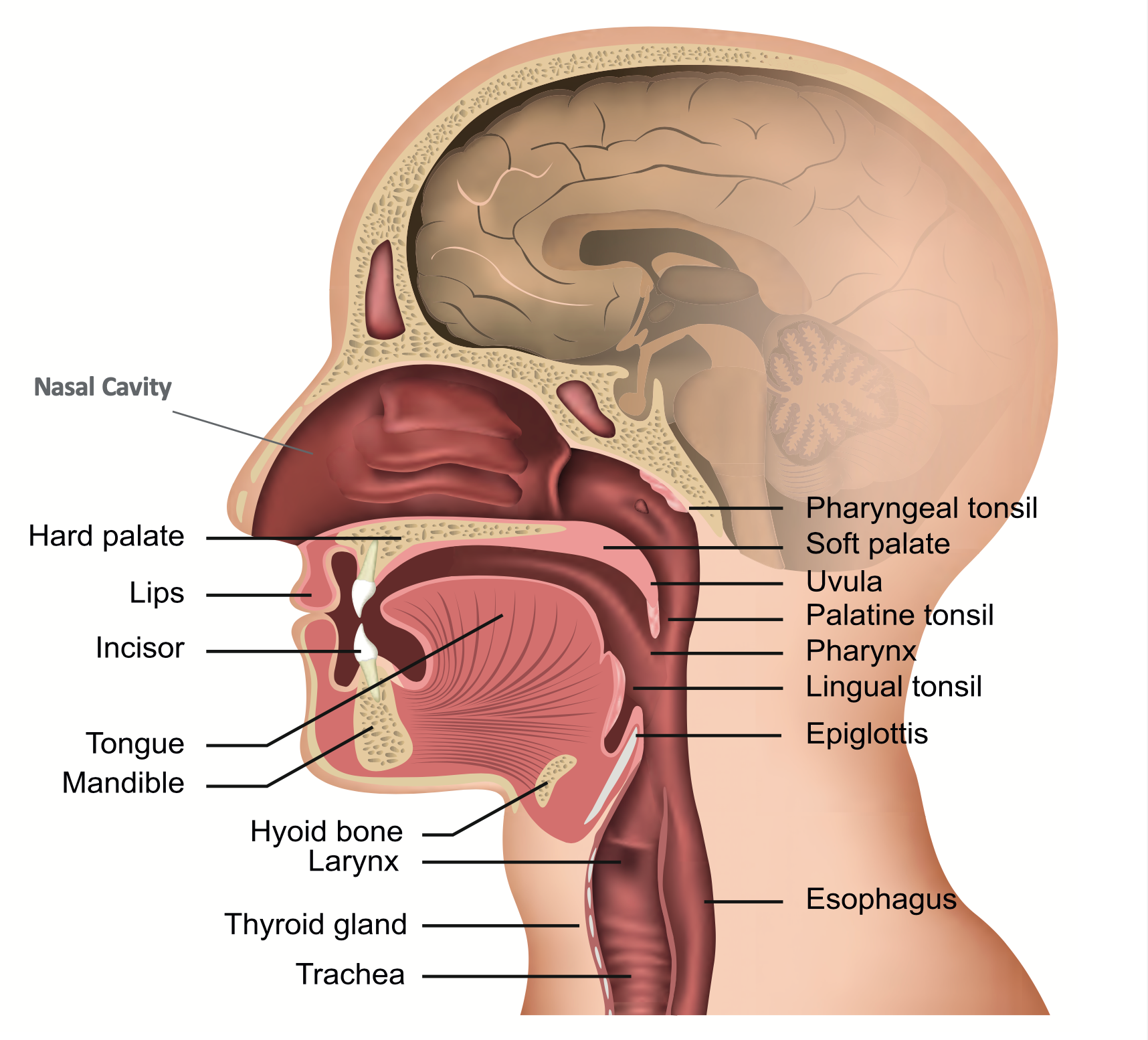
Figure 1. Oropharynx.
Let's proceed into the anatomy and dive deeper. We will refer to Figure 1 frequently because it is essential to understand better what we are looking at and what we are talking about in sleep apnea. In this cross-section of the oropharynx, we see the nasal cavity. I am going to point out a few areas here. In Figure 1, we see the soft palate, and if you go down a little bit inferior, you have the uvula, the pharynx, the epiglottis, and the base of the tongue. The tongue base looks like a "fan," which is the area we are concerned with. Of course, in Figure 1 there is no airway obstruction. Remember these areas, the uvula, soft palate, the tongue, the pharynx, and the epiglottis.
Obstructive Sleep Apnea Mechanism
We talk about the critical points on the mechanism of obstructive sleep apnea. Pharyngeal collapse occurs posterior to the tongue, uvula, and soft palate in the area from the posterior nasal septum to the epiglottis in Figure 1. This area has little bone or rigid support and mainly depends on muscle activity to maintain patency. In Figure 1, we did not see any bone. It is mainly muscle. The primary abnormality in patients with obstructive sleep apnea is an anatomically small pharyngeal airway resulting from obesity, bone, and soft tissue structures, or in children, tonsils, and adenoids. Remember when we were going through the history of sleep? In 1970, the Italian group noted that non-obese people dealt with sleep apnea. I would like you to plug that knowledge into your brain.
The tongue, epiglottitis, nasal septum, soft palate, uvula, pharynx, and we are speaking about these areas where sleep apnea occurs when you are asleep. During wakefulness, this leads to increased airflow resistance and greater intrapharyngeal negative pressure during inspiration. Mechanoreceptors located primarily in the larynx respond reflexively to this negative pressure and increase the activity of several pharyngeal dilator muscles, thereby maintaining airway patency while awake.
We have these muscles working while awake to keep the airway open. In Figure 1, the airway is completely open, and there are no obstructions. You can assume these mechanical receptors are working perfectly fine, and therefore, there is no collapse. But here is the kicker, since we are referring to obstructive sleep apnea, during sleep the reflex pharyngeal muscle activity that drives this neuromuscular compensation is reduced or lost, leading to reduced dilator muscle activity. Therefore, the airway is not going to stay open, ultimately leading to pharyngeal narrowing, intermittent or complete collapse.
During the subsequent apnea or hypopnea, hypoxia and hypercapnia stimulate ventilatory effort, e.g., fluttering your eyes, kicking, jerking, or even sitting up, and ultimately arousal from sleep to terminate the apneic event. Thus, the airway that requires reflex-driven muscle activation to maintain patency during wake may be vulnerable to collapse during sleep. This is the sleep apnea mechanism that is taking place. Depending on one's severity, the person will go in and out of these events throughout the night.
List of Disciplines
Many disciplines can help with OSA treatment. We have some important ones listed below.
- Physicians
- Internal medicine
- Psychiatrists
- Neurologists
- Pulmonologists
- Otolaryngologist (ENTs)
- Registered Dieticians and Nutritionists
- Respiratory Therapist
- Yoga instructor
- Dentist
- Physical Therapist
Internal Medicine
Internal medicine and primary care doctors are where it tends starts. You are thinking, let me see my primary care physician and see what is going on. See your primary care doctor first if you have questions about snoring, morning headaches, memory problems, or other signs of sleep apnea-gasping for air. This would be where the first line of defense, so to speak, you experience morning headaches, or you told you stopped breathing at night. They can, at times, help diagnose you and get you treated. In most cases, what they end up doing is referring to a specialist and letting the specialists manage your airway. Although this sounds like an excellent starting point, according to the Journal of the American Medical Association, in 2015, 25% of Americans did not have a primary care provider (Levine, 2020). The search was from 2015, and we can only assume that as time has passed those numbers may have increased. Many people may not be seeing their primary care physician, and 1 in 12 are walking around undiagnosed with sleep apnea, or 20 million Americans are dealing with sleep apnea.
Pulmonologist
After seeing an internal medicine doctor, you will be referred to a pulmonologist, a board-certified sleep doctor who knows all aspects of sleep and diagnosis. The main concern is that if we do not have a primary care doc, how do we get to the pulmonologist? These are all things I want our brains to be thinking about. How does this happen, and how do we do this? The pulmonologists may say, "You need to get a sleep test. It can be done in the sleep lab or a home sleep test." A sleep lab has a person there observing your sleep. You have different leads hooked up monitoring at different intervals while you sleep. Alternatively, you can take a home sleep test. A device with a pulse-oximeter placed on your finger, a thin wire is taped by your nose and mouth to monitor your airflow, and there is a band that goes around the chest to collect data on respiratory effort.
Treatment
The treatment usually comes from the pulmonologist or sleep doctor. Continuous positive airway pressure (CPAP) is the gold standard for OSA treatment. However, we have major concerns with CPAP compliance. The compliance rate is between 30 - 60%. Although I believe that 60% is a bit high, for various reasons as people complain of being claustrophobic or the convenience factor. Let's say, if you are traveling, you need to pack your CPAP on a piece of carry-on luggage. It would be best to have it with you on the plane because when you are flying, the worst-case scenario may be that your luggage does not land with you or is lost. Now you are without your device, which we know happens more often than we would like to, but most importantly, we want to get there safely. Then you have facial bruising. The mask may leave an indentation, and you would wake up with a third eye. We have to overcome these initiatives with our patients asking who needs to use CPAP and the various reasons for its use. There are certain side effects, but we try to encourage CPAP compliance for those who will benefit most from it.
Otolaryngologist
- Ear, Nose and Throat Doctors (ENT)
- Also called otolaryngologists, these doctors specialize in diseases involving the structures inside your head and face
My son had to see an ENT physician when he was four or five years old because he had some breathing issues at night and snored very loud. The ENT removed his tonsils and adenoids. ENT physicians can help if your airways are narrowed due to tonsils or tongue being large compared with the opening to your windpipe or if your airway is naturally small. The removal of tonsils and adenoids for children can be life-saving. Children dealing with sleep apnea are at risk of having difficulty concentrating, an increased chance of poor academic results, and even growth disturbances. School problems have been reported in multiple case series of children with OSA, and such findings may underscore more extensive behavioral disturbances such as restlessness, aggressive behavior, excessive daytime sleepiness, and poor test performances. We notice these effects may lead up to a diagnosis of ADHD before asking, Let's find out how the child is sleeping? The good thing is when you take the child to see an ENT and say, "Hey, this is what we are noticing." The ENT will say, "Let's take a look inside.” Then they look inside and say, "Wow, the tonsils are large, which could cause the problem. I would like you to record your child's sleeping and see what is happening." If deemed the case, an appointment to have the tonsils and adenoids removed is scheduled, which is sometimes a game-changer. Academic performance may improve, and the restless behavioral issues may start to mellow down because the child is now sleeping well.
Neurologists
Neurology is fascinating. As you age, your brain may not signal your throat muscles to stay rigid while you sleep, narrowing your airways. Your tongue may also relax excessively, affecting how much air you can breathe in. Neurologists focus on this and other ways your brain and nerves contribute to sleep apnea. Think about when you were 18 years old, if you grabbed the underpart of your tricep, how that muscle was probably solid. As we age, that tricep muscle begins to loosen. Unfortunately, the same happens with our brains. It may not send signals to the body or the brain saying, Hey, start breathing again, or realizing I am not breathing until I stop breathing. Neurologists may complete diagnostics to determine if the individual does or does not have any malfunctions affecting the brain and the sensory-motor pathways associated with sleep.
Psychiatrists
Figure 2. Image of Brain.
You think about the comic books you may have read when you were 12, 13, or 14 years old. People often have favorite memes, cartoons, and theme songs. We have all these things inside our brains referring to Figure 2. I enjoyed math and science as a younger child. We have had a lot over the past couple of years in mental health. We have things like depression and anxiety under the umbrella of mental health that are starting to rise. Psychiatrists or other mental health professionals can play a vital role in helping somebody deal with sleep apnea. Sometimes, behavior change alone can resolve or support treatment of sleep apnea. Losing weight, sleeping on your side, and quitting smoking may help keep your airways open. Behavioral health experts can help you create a plan to modify these factors and get a good night’s rest. These professionals can also help you manage the effects of poor sleep on mental conditions, including depression, anxiety, and bipolar disorder. These experts can then create a plan that modifies some of these health behaviors that affect them, preventing them from getting enough sleep.
Anxiety and OSA
- most common mental illness in the U.S.
- affecting 40 million adults in the United States age 18 and older, or
- 18.1% of the population every year
Anxiety disorders develop from a complex set of risk factors, including genetics, brain chemistry, personality, and life events. We know that there is a link between obstructive sleep apnea and anxiety. As we go through the process, when we think about the mechanism we have talked about when someone is experiencing a sleep apnea event, they have decreased in oxygen consumption and an increase in carbon dioxide. We have this poisonous gas (carbon dioxide) in our brain that is just there, happening multiple times throughout the night. Then, the person has arousal. It is almost like you are being scared by a bear. Imagine that. Being scared by a bear and your heart is racing. You are not able to get this restorative sleep. Your brain and your heart are stressed.
Suppose someone is dealing with anxiety and obstructive sleep apnea that is not managed because we have 20 million Americans undiagnosed. In that case, anxiety affects 40 million adults in the United States. Now we start putting this all together. People with anxiety disorders are 3 to 5 times more likely to go to the doctor. They are six times more likely to be hospitalized for psychiatric disorders than those who do not suffer from anxiety disorders. Anxiety disorders are highly treatable, yet only 36.9% of those suffering receive treatment. The question is, how many of them are screened for sleep apnea? That is something we do not know. We know that there are 1 in 12 or 20 million people who are undiagnosed with sleep apnea. We need to start thinking, that is the fight we are up against to see how we can spread the word about sleep apnea. How can we help to treat people? Just a thought of mine, maybe we start seeing these numbers when people dealing with anxiety issues start to come down.
Surgeons
If your sleep apnea does not respond to treatments like weight loss, breathing machines, or dental devices, you might need surgery. For most people, that is the last resort to have anything cut on, but surgeons play a critical role because there are some treatments that people will not respond to a CPAP. It would help if you had other treatments that could help manage one with sleep apnea. The type of surgery you have will depend on the cause of your apnea. In some cases, a surgeon can perform a simple procedure to shrink the tissue in your mouth or throat that is blocking your airway. Other times, more extensive surgery is required to cut away from your tonsils or other extra tissue. For these procedures, you will usually receive general anesthesia, spend some time in the hospital, and have throat pain for a week or two afterward. Of course, this is something the individual will need to have a conversation with the surgeon to find out the benefits of the risk-reward analysis on undergoing any procedure as it relates to surgery.
Yoga
Yoga can play a significant role in treating someone with obstructive sleep apnea. Yoga is an ancient Indian practice of mental and physical exercises, postures, movements, and breathing techniques that sustain the healthy living of the body and the mind. Yoga incorporates various exercises of breathing, oropharyngeal structures, and facial expressions. We deal with breathing and pharyngeal structures in sleep apnea. Going back to our Figure 1 diagram, we saw where sleep apnea occurs and the structures are primarily muscle. If we take into account practicing yoga, we can strengthen these muscles. Yoga is an added treatment that can be done for sleep apnea and not just fall on one team member to dictate. The physiological effects of yoga are comparable to international physiotherapy recommendations in OSA treatment.

Figure 3. Image of yoga position.
Figure 3 illustrates a person sitting upright, focusing on their posture. They are in a relaxed state, and they are upright. It looks like the neck's elongated. All the things that can help towards treating somebody with sleep apnea. I think the picture says a thousand words about yoga and its place in treating someone with sleep apnea. I am not saying all you need for sleep apnea is yoga, but yoga benefits someone who has sleep apnea.
Registered Dietician and Nutritionist
OSA and several of its co-morbidities have significant nutrition-related implications.
- Obesity
- Type 2 diabetes
- Hyperlipidemia
- Chronic obstructive pulmonary disorder (COPD)
- Resistant hypertension
- Asthma
- Chronic kidney disease (CKD)
- All have nutritional involvement in varying degrees
Registered dieticians (RD) and nutritionists play a crucial role in treating OSA. OSA and several of its co-morbidities have significant nutrition-related implications. Research from Morrow (2020) concluded in 2017 and 2018, 42% of the US population is dealing with obesity. When we think of type two diabetes, hyperlipidemia, COPD, resistant hypertension, these diseases are often related to someone taking three or more blood pressure medications to control their hypertension. You could ask, do we give them more medication? Are they suffering from sleep apnea, or can we at least rule it out? We know most people do not want to take more medication, but it would be beneficial to find out by scheduling a sleep test and seeing if there are some underlying issues. Often, an indication someone is dealing with sleep apnea. Additionally, Morrow (2020) found asthma and chronic kidney disease have nutritional involvement in varying degrees. The study estimated that 40 to 70% of obese individuals are diagnosed with sleep apnea. Obesity is a major focus in nutrition research and OSA due to the high incidence of co-morbidity. Low-carbohydrate dietary approaches and Mediterranean-style meal patterns are beneficial in OSA and the effects may be beyond weight loss alone. Additionally, high fat intake was associated with daytime sleepiness and apnea and hypopnea index (AHI). AHI refers to how often the individual stops breathing or has reduced breathing events throughout the night. These individuals tend to be more sleepy during the daytime. High alcohol intake is related to the severity of OSA and low fiber intake is present in OSA patients. The big push here is if someone is dealing with OSA, let's try to reduce their alcohol intake.
Many of us eat out at restaurants. Sodium restriction has been explored in the treatment of OSA. Dietary salt has been associated with the severity of OSA in individuals with hyperaldosteronism and resistant hypertension. Restricting sodium to mitigate fluid retention in males with severe sleep apnea resulted in a limited decrease in apnea episodes. The fight we are up against is the stereotypical OSA person who looks big and male over 50 years old. Remember, we do not want this aged image of a male dealing with sleep apnea. In 1970, research found non-obese individuals were dealing with sleep apnea. Morrow (2020) determined the dietary manipulation of macronutrient distribution in calorie content demonstrated effectiveness in decreasing OSA severity. Dietary treatment alone and in conjunction with exercise may effectively improve the severity of OSA. We are working on this mind shift. We exercise and we alter our diet. if we can work on these approaches, we can help to improve our outcomes with OSA treatment.
Dentist
These medical professionals do more than fill cavities. Some dentists have special training in treating sleep-related breathing disorders, including sleep apnea. They can fit you with a custom fit oral device that moves your lower jaw forward, making breathing easier. Usually, a dentist will work with a board-certified sleep specialist to manage your care. The physician will oversee your treatment, while the dentist will make changes to your oral device as needed to improve your symptoms. After a dentist complete's his assessment, they can say this individual may have sleep apnea. Although the dentist cannot diagnose only by looking, the dentist may think it is good to get a sleep test, and you need to be seen by your primary care physician.
Oral Appliance
At this point, the individual completes a sleep test. The results confirm sleep apnea. Guess what? You get to wear CPAP. The individual says, “I do not think so, are there other treatments?” The person may be worried about claustrophobia, traveling, or carrying a large device which increases the likelihood of not following through with treatment. Your dentist can talk about other treatments with you. They can fit you with a custom-fit oral device that moves your lower jaw forward, making breathing easier. Usually, a dentist will work with a board-certified sleep specialist to manage your care. The board-certified sleep doctor helps make sure it is working effectively for you. The physician will oversee your treatment, while the dentist will make changes to your oral device as needed to improve your symptoms. Now, we have this happy patient, an individual who is not having to wear a mask, and when you travel, you can put this in your purse, bag, or pocket.

Figure 4. Example of an oral appliance.
Figure 4 is an example of an oral appliance for sleep apnea. You place the oral appliance inside your mouth, and the top and lower teeth help pull your lower jaw forward or stabilize it, thereby opening your airway. It is not a large appliance. It helps to serve two purposes, sleep apnea and someone grinding their teeth, which can lead to more dental work and more money, which we want to avoid if possible.
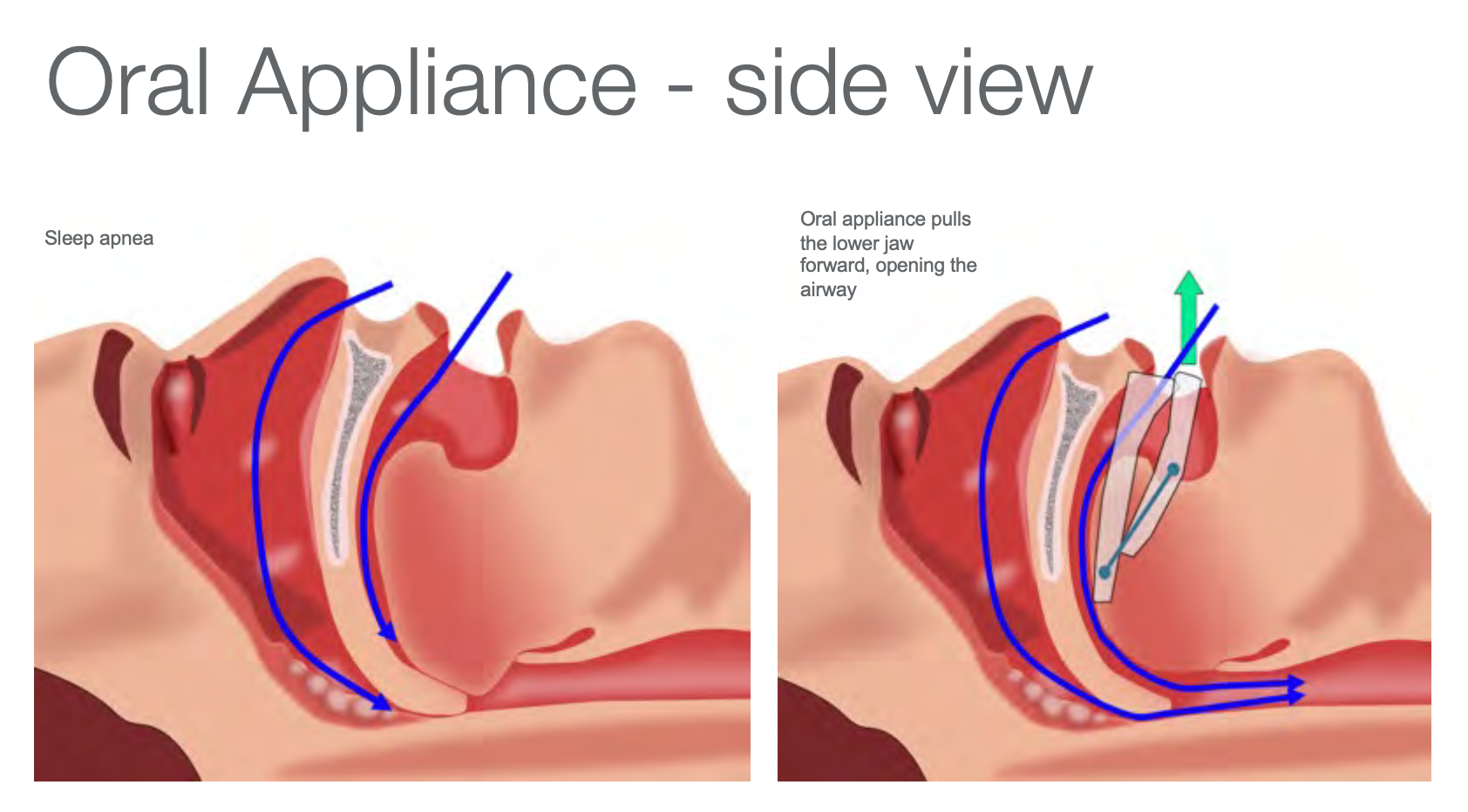
Figure 5. Lateral view of an oral appliance.
Figure 5, the image on the left illustrates the lateral view of the oropharynx without the oral appliance inserted. You see the air (blue arrows) is not getting in during sleep apnea. The tongue has collapsed, and the air cannot go down. What is happening is that the person cannot expel oxygen, increasing carbon dioxide. The image on the right illustrates a custom-fit oral appliance that is helping to advance the lower jaw forward and hold it. We can see the oxygen going in (blue arrows) and carbon dioxide going out (green arrow) during sleep- a restful night adds to a healthier individual.
The Stages of Obstructive Sleep Apnea
Let's review the different stages of OSA.
- Normal: <5 per hour
- Mild: 5-15 per hour
- Moderate: 15-30 per hour
- Severe: >30 per hour
Is It Normal to Stop Breathing at All?
One thing we know is that oxygen is essential for living. So is it normal to stop breathing at all? I will let you decide.
Prevalence of Obstructive Sleep Apnea
- Adults ages 30-70 in 2016
- 13% of men have moderate to severe OSA
- 6% of women have moderate to severe OSA
- The numbers as of 2016, 29.4 million
- Undiagnosed: 80%, 23.5 million
- Diagnosed: 20%, 5.9 million
The Gold Standard
The gold standard is the CPAP. We know that it works. Then we ask ourselves, what if the gold standard is sitting on the dresser because you cannot wear it? It causes irritation, or you are worried about getting tangled up with the tubing while sleeping. Is it then the gold standard?
What Becomes of the 40%?
- 5.9 million people diagnosed with OSA
- 85% given CPAP (5 million)
- Assuming 60% are compliant with their CPAP (3 million)
- 40% are not compliant (2 million)
For certain, they are not getting enough sleep. Let's say roughly 85% are provided with CPAP treatment. That is 5 million people. If we take the higher compliance number, 60% are compliant with their CPAP, which is 3 million people. If 40% are not compliant, then there are 2 million people who are not compliant with their CPAP.
Alternatives to CPAP
- Custom-fit oral appliances
- Inspire-stimulation of the hypoglossal nerve
- Surgery-repositioning of the lower jaw
There are several alternatives to CPAP. We have spoken about the custom-fit oral appliance. Another alternative is Inspire, which you may see in commercials. Inspire is a minor surgical procedure similar to how a pacemaker is placed, though instead of stimulating the hypoglossal nerve, it stimulates the nerve within the tongue. One more option is surgery to reposition the lower jaw. Some individuals may not want to be involved in any surgeries, and from this point, we dive further into custom-fit oral appliances.
Benefits of Custom Fit Oral Appliances
- Decrease Daytime Sleepiness
- Reduction of AHI
- Reduction of snoring
- Improvement with diastolic and systolic blood pressure
The oral appliance reduces AHI, leading to decreased oxygen desaturation, diastolic and systolic blood pressure improvement for many patients with high blood pressure and sleep apnea. About half of the United States population have high blood pressure, many of whom are undiagnosed. Those using the oral appliances would want to know how this will affect my blood pressure? There is data showing it improves your blood pressure. Another issue it helps reduce is excessive daytime sleepiness, affecting people when they are driving. Motor vehicle accidents are increasing, and we need to handle this. I have had several people tell me, "I cannot sleep with my spouse because they snore. I cannot sleep because my house is shaking from how loud they snore. This creates a big issue where spouses cannot sleep together in the same room. A big kicker here is the reduction of snoring as a benefit of using an oral appliance.
Mean Disease Alleviation
Mean Disease Alleviation (MDA) refers to the potential of treatment or a combination of treatments to effectively decrease the likelihood of developing serious consequences of co-morbid conditions associated with OSA. Here is a formula that I want us to look at closely.
- MDA= (adjusted objective compliance x therapeutic efficacy)/100
This is how to calculate MDA or mean disease alleviation. You have your adjusted objective compliance times your therapeutic efficacy divided by 100. Objective compliance is what the patient admits to doing. For example, the patient must wear their CPAP for at least four hours out of the eight-hour period. If not, there is "big brother watching" and they can come and remove CPAP from you. You may not be happy.
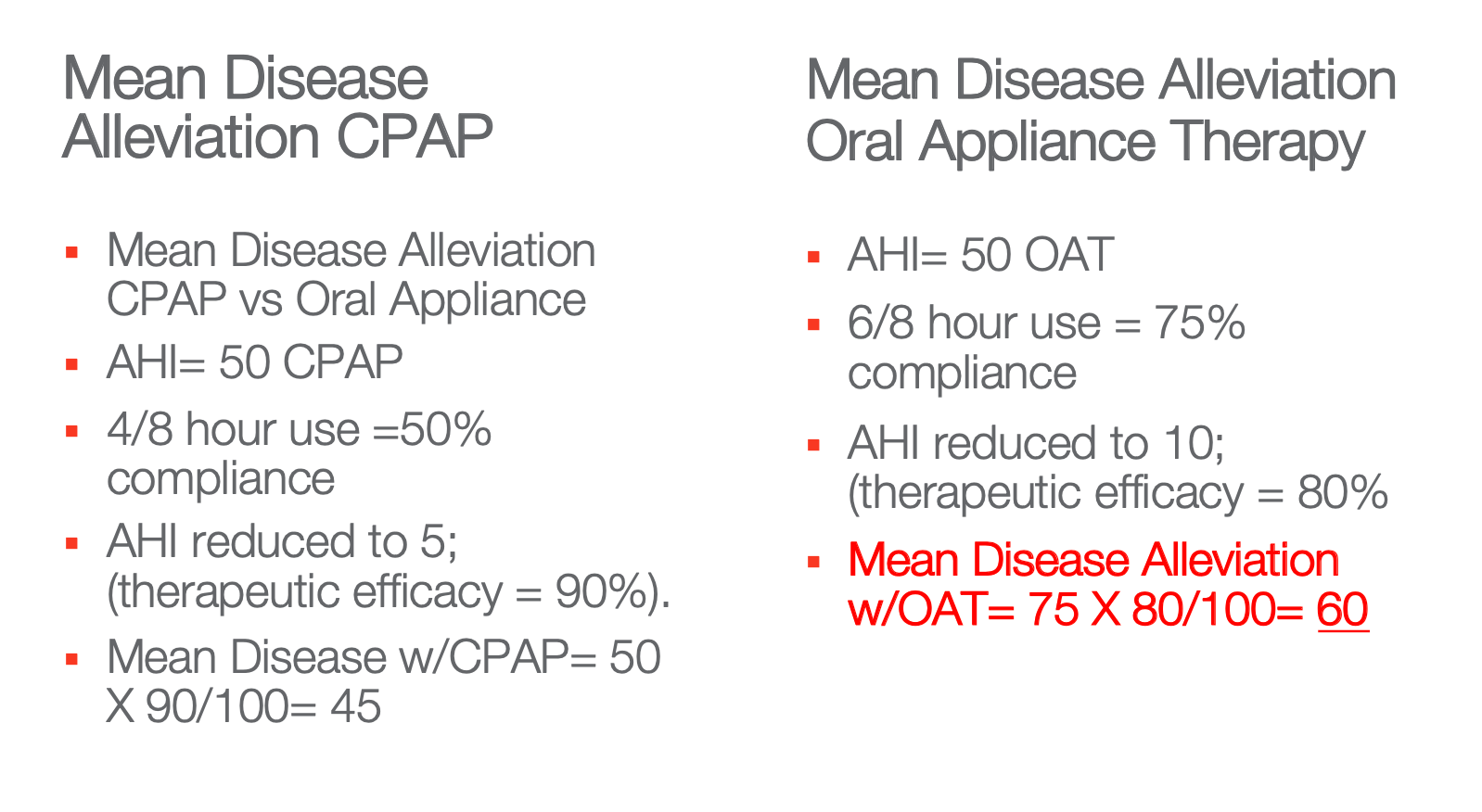
Figure 6. Mean Disease Alleviation comparison.
Figure 6 compares mean disease alleviation between CPAP and oral appliance therapy. Looking at the left column, let's say an AHI with the CPAP is 50. The person wears their CPAP for four hours out of the eight hours, the usage comes down to 50% compliance. AHI is reduced to five, which shows a therapeutic efficacy of 90%. Now, this is a matter of plugging in numbers, so compliance of 50 multiplied by a therapeutic efficacy of 90, divided by 100, gives us 45% mean disease alleviation with CPAP use. On the right-hand side of the column, this individual tends to be more compliant with the oral appliance. On average wearing, about six hours out of the eight hours gives us about 75% compliance. Plugging in the numbers, gives us 60% mean disease alleviation. The information tells us the more you wear the oral appliance, the greater the mean disease alleviation compared to the CPAP.
We start to think, gold standard sitting on the shelf vs. oral appliance being used, which one would you prefer? Phillips et al. (2013) found in the short term, health outcomes in patients with moderate to severe OSA were similar after treatment with CPAP and mandibular advancement devices. Likely explained by the greater efficacy of CPAP being offset by inferior compliance, relative to mandibular advancement devices. These findings strongly challenged current practice parameters recommending mandibular advancement device treatment be considered only in patients with mild to moderate OSA. It is showing that the mandibular advancement device is a good treatment for not only mild to moderate but it should be considered for your patients with severe OSA. According to the American Journal Of Respiratory and Critical Care Medicine, long-term comparative effectiveness studies between CPAP and mandibular advancement devices include objectively measured treatment compliance needed to define treatment strategies for patients with OSA. Something to think about custom-fit oral appliances, mandibular advancement devices, and CPAP is not the only treatment for OSA. According to the American Academy Of Sleep Medicine further findings in this context suggest that the clinical role of mandibular advancement device treatment should be extended beyond the currently accepted mild to moderate OSA range. We should think about and understand this.
Physical Therapist
Physical therapy can be prescribed for clinical improvement of sleep apnea for patients with OSA. Here is a fascinating study involving a larger sample. In the Journal of Clinical Sleep Medicine, Paruthi et al. (2016) reported data showing the impact of aerobic exercise on sleep-disordered breathing on 155,448 individuals as part of the extensive Ontario Health Study. This large population-based study examines various health-related behavior, medical history, demographic factors, and health service utilization. This investigation examined exercise, behavior, and physician-diagnosed with OSA. These investigators found that physical exercise was associated with a decreased prevalence of OSA independent of generally known risk factors, including body mass index. Increased total physical activity, vigorous-intensity activity, and walking were all associated with a decreased prevalence of OSA. Hence, as kids, they used to tell us, "Hey, go out and exercise." We are seeing it wrap back around, the importance of exercise. We come home from work, maybe tired, and it is a matter of getting out, knowing that we are helping to mitigate some of these other issues that could arise or that we are dealing with. The physical therapist can help support and incorporate exercise into the individual's daily routine.
Respiratory therapist
A respiratory therapist helps patients who have trouble breathing. Respiratory therapists work under the direction of doctors and treat a range of patients, from premature infants whose lungs are not fully developed to older adults with lung disease. I look at respiratory therapists as life-givers. Respiratory therapists give patients oxygen, manage ventilators, administer drugs to the lungs, and so much more. I thank you for the work that respiratory therapists are doing, especially given this time with COVID-19
References
Thirty Years of CPAP. A Brief History of OSA. (2011). Res Medica Journal of the Royal Medical Society Clinical Newsletter, Issue 14.
Aserinsky, E., & Kleitman, N. (1953). Regularly occurring periods of eye motility, and concomitant phenomena, during sleep. Science, 118(3062), 273-274.
Dement W. C. (2005). History of sleep medicine. Neurologic clinics, 23(4), 945–v.
Gozal D. (2008). Obstructive sleep apnea in children: implications for the developing central nervous system. Seminars in pediatric neurology, 15(2), 100–106.
Kleitman, N. (1982). Basic rest-activity cycle—22 years later. Sleep, 5(4), 311-317.
Levine, D. M., Linder, J. A., & Landon, B. E. (2020). Characteristics of Americans With Primary Care and Changes Over Time, 2002-2015. JAMA internal medicine, 180(3), 463–466.
Morrow, E. A. (2020). Medical Nutritional Therapy in the Management of Obstructive Sleep Apnea. Journal of Nutrition and Dietetic Practice.
Paruthi, S., et al. (2016). Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(6), 785–786.
Phillips, C. L., et al. (2013). Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. American journal of respiratory and critical care medicine, 187(8), 879–887.
Stepnowsky, C. (2019). Multidisciplinary Approach to Sleep Apnea Management. Medical Research Archives, 7(7).
Todman, D. (2007). A History Of Sleep Medicine. The Internet Journal of Neurology, Volume 9 Number 2.
Citation
Imo, K. (2022). A Team approach for sleep apnea. Continued.com - Respiratory Therapy, Article 137. Available at www.continued.com/respiratory-therapy
