Editor's note: This text-based course is an edited transcript of the webinar, Reducing the Stigma of HIV/AIDS, presented by Sara Pullen, DPT, MPH.
Learning Outcomes
After this course, participants will be able to:
- List transmission routes and basic terminology used for HIV.
- State the most common forms of stigma experienced by people living with HIV.
- Describe three ways to reduce HIV-related stigma in the school, daycare or childcare learning environment.
HIV/AIDS Definitions
- HIV: Human Immunodeficiency Virus. Progressive failure of the immune system that allows life-threatening opportunistic illnesses to thrive. Untreated, HIV progresses to AIDS.
- AIDS: Acquired Immunodeficiency Syndrome. Immune system is severely compromised and vulnerable to opportunistic illnesses.
- PLHIV – People Living with HIV
- ART – Anti-retroviral therapy, the life-saving medication used to control HIV
- CD4+ (“T-cell”): type of white blood cell that fights infection
- Move throughout the body identifying/destroying viruses and bacteria
- HIV binds to and enters CD4 cells à makes copies of itself à gradual decline of CD4 cells and immune system
Let's get started with some basic definitions. HIV stands for the Human Immunodeficiency Virus. Let's break that down a bit. We all know what human means. Your immune system is what keeps you healthy and if it's deficient or lacking it's an immunodeficiency. Virus is another term we all know as well. In lay terms, this is a progressive failure of the immune system that allows life-threatening opportunistic illnesses or infections to thrive. If it's left untreated HIV will progress to AIDS.
AIDS is the Acquired Immunodeficiency Syndrome. Acquired means to get something, immunodeficiency we just talked about, and syndrome is a collection of different things, such as symptoms or issues. At this point the immune system is severely compromised and vulnerable to opportunistic illnesses.
Over the years there have been several ways to refer to people living with HIV. Back in the 80s, people would say AIDS victims or AIDS patients, but that’s not used much anymore. Now in the scientific literature and in AIDS care what we really hear most up is people living with HIV. Throughout this course, I'll be saying PLHIV. You’ll now know that I'm referring to people living with HIV. The reason this term is being used with research and with AIDS activism is that we want to put the person first. We don't want to put the disease first. You wouldn't say, “A diabetes victim” for example, you'd say, “Someone with diabetes.” It's a person first and they happen to be living with HIV because HIV and AIDS are not a death sentence anymore.
ART stands for Anti-retroviral therapy. A is the type of virus HIV is, which is a retrovirus. You can have different kinds of viruses, such as the norovirus, the stomach bug nobody wants to get. Antiretroviral therapy means you're going against the virus and are trying to kill it. Therapy medication is a life-saving medication used to control HIV.
CD4 cells are also called T-cells. They are a type of white blood cell that fights infections. We all have CD4 or T-cells in our body. That's a major part of our immune system. In a healthy body, our T-cells move throughout our body, identifying and destroying viruses and bacteria. If you touch a doorknob, touch your face and a bacteria or virus gets into your system, these T-cells are constantly zooming around your system and they identify what's not supposed to be there and they kill it and destroy it.
In the case of HIV, HIV binds to and enters CD4 cells and it makes copies of itself which leads to a gradual decline of CD4 cells in our immune system. Take a moment and make a fist in front of you. Your fist represents a CD4 cell. HIV would be like a little marble (the virus) coming into your fist. Instead of your T-cell (or CD4 cell) actually destroying the virus, the HIV virus knows how to get inside that T-cell. Your fist is the T-cell and the marble comes zooming into your fist. Once the virus is inside the T-cell it makes copies of itself. Let's say one HIV molecule gets in there and then five come out. Now you have not only one, let's just say a piece of an HIV virus trying to wreak havoc, but you have five and then those five get into a cell and they replicate. The issue with HIV is that those HIV viruses keep making copies of themselves and eventually your immune system just can't keep up, which causes a decline of the CD4 cells and the immune system.
How is HIV measured?
HIV is measured in terms of CD4 cells. You may have read about or heard people with HIV talking about T-cell counts. Typical, normal, healthy adults have about 1,500 T-cells in their body. People with HIV have a lower number. If you have AIDS you usually have less than 200 T-cells. Everyone has T-cells and a CD4 count but in healthy people, they have more because HIV hasn't destroyed them.
Another way that we measure HIV is called a viral load. That's the measurement of how many HIV copies are in a blood sample. Remember we have that fist (the T-cell) and the marble of the virus coming in and replicating itself. That's how many copies are in a blood sample. Clearly the lower the viral load the better.
Viral suppression is the goal. The goal is for it to be undetectable. This means that if you have a blood test and they cannot detect any copies of HIV in your system you’ve met the goal of the virus being undetectable. You may hear people saying something like, “That person is undetectable.” That's the goal as long as there's no cure or a vaccine. As of now, once you have HIV you're never cured of it. We hope that we can someday say differently, but as of now, the goal is to suppress the virus. The goal is to have the medicine that basically shuts down the HIV. Even if someone has an undetectable viral load they are not able to transmit the virus. So, in other words, the goal is to get the virus suppressed but unfortunately, it doesn't mean that you're free of HIV.
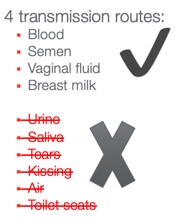
Figure 1. Transmission routes for HIV.
What are the four transmission routes for HIV? In figure 1 you can see a green check next to four bullet points: blood, semen, vaginal fluid, and breast milk. Those are the four ways body fluids with HIV can pass from one person to another. Below that, you'll see an X. Next to this list are ways that HIV cannot be transmitted. They are crossed out as a reminder that they are not ways to transmit HIV. It cannot be transmitted through urine. It cannot be transmitted through saliva, so not through kissing or through sneezing if someone sneezes on you. It can’t be transmitted through tears, through the air, or through toilet seats. When I give talks, people often laugh when I say this. I’ve noticed that it depends on how old they are. People who are a little older and have been doing HIV work forever don't laugh because they distinctly remember that people thought you could get it through toilet seats. We now know that you can't.
Stages of HIV Infection
Let's talk a bit about the stages of HIV infection.
- Acute HIV Infection (weeks 2-4 post infection):
- Develop flu-like symptoms; “worst flu ever”
- Large amounts of HIV in the blood and immune system
- Greatest transmission risk
- Chronic HIV Infection:
- HIV reproduces at low levels
- People may be asymptomatic but still contagious
- With proper treatment – life expectancy = general population
Acute HIV infection occurs right when someone gets infected, whether through unprotected sexual contact, through a needle, or any of the other ways I just discussed. People report developing flu-like symptoms and have described it as the worst flu ever. You can't move and you feel awful. There's a large amount of HIV in the blood and the immune system and you're at the greatest transmission risk. When someone's infected with HIV and those HIV copies are going berserk in that person’s body, they're replicating and attacking all the T-cells, which means the immune system goes down and people feel extremely ill. Then they feel better.
With a chronic HIV infection, the HIV reproduces at low levels. People may be asymptomatic, meaning no symptoms, but they are still contagious. With proper treatment, life expectancy is equal to the general population. In 2013 there was a major announcement that once someone's viral load becomes stable and is considered undetectable, their life expectancy is equal to the life expectancy of their HIV negative peers. That was a huge scientific discovery.
Current HIV Statistics
- 39,782 new HIV infections in 2016 in USA
- Estimated 1,123,000 PLHIV by 2016
- 1 in 8 HIV+ people are unaware of their infection
- Among 13-24 year olds, 51% don’t know they are infected
- Highest risk communities: economically disadvantaged urban areas in the U.S., the South, MSM (men who have sex with other men) and African-Americans (12% of U.S. population; 41% of HIV infections), Geriatric population (55 or older) – 26% of all HIV infections in U.S.
Current HIV statistics ebb and flow and change depending on treatments and research. There were 39,782 new infections in 2016 in the USA. These are people who were not positive before and already had it. This is people who were newly infected in 2016. Think about that for a second. Nearly 40,000 people in this country were infected by HIV in the US in 2016.
The Centers for Disease Control (CDC), the World Health Organization, and National Institutes of Health put out new statistics about every two years. We should be getting 2017 numbers pretty soon. It's estimated that 1,123,000 people were living with HIV in the US in 2016. About 40 thousand were newly infected but about 1.1 million people were living with HIV in 2016.
The third bullet point is alarming. One in eight HIV-positive people is unaware of their infection. For people with HIV, one in eight are unaware of their infection. Among 13- to 24-year-olds, 51% don't know they're infected. About one out of every two people age 13 to 24 years old who have HIV don't know they're infected. If this is sending up your alarm bells it should. This is an extremely high-risk group and this spans people who were having sex with the same sex, with the opposite sex, heterosexual, homosexual, it doesn't matter. People age 13 to 24 years old is a major high-risk group.
The highest risk communities are those that are economically disadvantaged. This includes poor areas in the urban areas of the US, especially in the southeast. People talk about the Bible Belt, which includes Georgia, Alabama, South Carolina, and North Carolina. This area is also sometimes referred to as the stroke belt because cardiovascular disease is so high. Among researchers, we refer to this area as the AIDS belt because there are an incredible amount of HIV infections here too.
African Americans comprise about 12% of the US population but about 41 percent have HIV infections. The geriatric population, which includes people 55 years or older, represents 26% of all HIV infections in the U.S. What we're finding is that people 55 years and older are not concerned about pregnancy so they’re often not worried about protection at all.
HIV in Children and Adolescents
Let's talk about HIV in children and adolescents. HIV can pass from a mother with HIV to her child during any time of pregnancy, childbirth, or breastfeeding and that's known as perinatal transmission. In the U.S, most cases of HIV diagnosed in children under 13 are due to mother-child transmission. In other words, mothers that did not know they had HIV when they were pregnant and gave birth ended up having a baby with HIV. The CDC reports that 122 cases of HIV were diagnosed among children younger than 13 in 2016. That's really encouraging that there was such a low number, but it should be zero. It's also encouraging that people are pretty aware of their status and HIV testing during pregnancy is standard as well for women.
The CDC recommends that all women who are pregnant or planning to get pregnant take an HIV test as early as possible before and during every pregnancy. If a woman tests positive and takes her HIV medicine daily as prescribed throughout pregnancy, labor, and delivery and gives HIV medicine to her baby for four to six weeks after delivery, the risk of transmitting HIV to the baby can be as low as 1% or less.
In 2016 or 2017 a baby was born with HIV and the HIV was treated. The baby later came back for testing and it appeared that there was no more HIV. It appeared that it was not even undetectable but the baby was actually “cured.” This was a huge scientific breakthrough. Unfortunately, the mother did not bring the baby back in to stay on her medications and the baby came back about six months later and had full-blown HIV again. The lesson here is that when a woman tests positive for HIV it's not a lost cause. The chances of the baby actually being born with HIV is 1% or less if the mom takes the medication and the baby is given the medication for about 1 or 2 months after he or she is born.
HIV Treatment
For babies living with HIV, starting treatment early is important because the disease can progress much more quickly in children than adults. It's very important for babies when they're born positive, to begin that treatment right away. Providing antiretroviral therapy (ART) early can help children with perinatal (mother-to-child) HIV live longer healthier lives.
Youth ages 13 to 24 are among high-risk categories and accounted for one in five new infections in 2015. Remember that about 20% of all new infections are among people this age group and about half people with HIV in this age group don't know that they have it.
HIV-Related Stigma
- Stigma: a mark of shame or discredit
- HIV-Related Stigma: prejudice, negative attitudes, and abuse directed at PLHIV
- Discrimination: the practice of unfairly treating a person or group differently from other people or groups of people
- Roughly 1 in 8 people living with HIV are denied health services because of discrimination.
- Stigma and discrimination also make people vulnerable to HIV (i.e. not getting preventive care).
What is stigma? Stigma is defined as a mark of shame or discredit. An example is to say that what you have or what you did is shameful and you're really not valuable. We're discrediting you. HIV-related stigma is prejudice, negative attitudes, and abuse directed at people living with HIV. Discrimination is the practice of unfairly treating a person or group differently from other people or groups of people. Discrimination we've all heard of and can include racial discrimination, sex discrimination, or age discrimination. If you think about this in the context of HIV, it would be unfairly treating a person with HIV or a group of people with HIV differently from other people who did not have HIV.
Roughly one in eight people living with HIV are denied health services because of discrimination. Stigma and discrimination also make people vulnerable to HIV. In other words, if someone is in a high-risk category for HIV but they're afraid to tell their doctor or they're afraid to talk about it because of the HIV stigma, they're more at risk for getting it. We've had situations at our clinic of teenagers saying, “Well I knew I was attracted to other men” or “I knew that I was sexually active with my girlfriend or boyfriend but I couldn't talk about it” or “I didn't want to talk about with anybody.” Then obviously they're not going to be wearing condoms or talking to anyone about their risk category and that can make them vulnerable to HIV.
People most at risk for HIV face stigma and discrimination based on various factors. These include:
- Perceived or actual health status
- Race
- Socioeconomic status
- Age
- Sex
- Sexual orientation
- Gender identity
- Other grounds
People face stigma and discrimination based on various factors, so if you think about people who are low socioeconomic status, men who have sex with other men, or people of color, they’re facing stigma based on completely something different than HIV. If someone is coming from a racial minority group or is extremely poor or is a man who has sex with other men, those people would be at risk categorically for HIV but they're already facing discrimination because of this. This makes them more at risk for HIV.
People living with HIV can face stigma in many settings, including home, work, and educational settings. I have a physical therapy clinic and HIV clinic here in Atlanta, Georgia where I live. There are 6,000 patients enrolled and it is a full-service clinic.
I’m going to share some examples of some of my patients who have faced stigma in the home. I can't even count the number of patients I've had who said they were diagnosed with HIV and may be kicked out of their house. This includes teenagers who were either diagnosed with HIV or were gay and their family kicked them out and they're on the streets and they contract HIV. I've had women who find out that they were HIV positive when they were pregnant and their husbands or male partners who infected them in the first place kicked them out of the house. Think about that for a second. A woman is pregnant and she's only ever had sexual contact with one person, her husband or her male partner. He kicks her out or abuses her as opposed to getting himself tested or supporting her. That's an example of home stigma.
Here are a couple of examples of work stigma. Sometimes a person with HIV will need to take their medication once a day, sometimes three times a day, and sometimes more. If it’s more than two times a day, they may have to take the medicine at work. People may ask what they are taking medicine for. The person with HIV may have a fear of stigma of disclosure. When I used to work in a hospital, every time you went to employee health they would ask if you are HIV positive along with if you smoke. We should normalize the way we ask people about HIV because there is such a stigma against it. People often say they don't want to disclose their HIV because they’re afraid they’re going to get fired. Unfortunately, even in this day and age, in non-discrimination policies, HIV status or even health status is not always there. In terms of non-discrimination policy, sometimes there is very little protection. Another thing to think about is workplace transmission. I often get asked if I’m scared of getting HIV from my patients. We’ll talk about that soon.
An example of educational stigma might be elementary school children who have HIV. Sometimes they still have to take their medicines when they're a little older. The school nurse would be the one to give out that medication so the school nurse would need to know about those kids with HIV. Just like any other profession, there are great ones and there are not great ones. Thinking about a child with HIV, certain people would need to know and if those people had real HIV stigma discrimination then that could make things extremely awkward for that little child who is just trying to stay healthy.
Why does HIV-related stigma still exist?
HIV-related stigma is based in fear surrounding the HIV epidemic in the 1980s and still persists today. I have colleagues at the AIDS clinic who were working in the hospitals in the 1980s when HIV was first coming out and nobody knew how it was transmitted. People didn't know if it was transmitted through the air or on toilet seats or through handshakes or hugs so there was a lot of fear because people didn't know how it was transmitted.
This historical fear plus many other reasons means that people still have a lot of false beliefs. One of those is that HIV and AIDS are always associated with death and think it’s a death sentence. Another false belief is that HIV is associated with behaviors that some people discriminate against such as same-sex relationships, IV drug use, or sex work. My experiences and the literature tell us that everyone's at risk for HIV. It’s not just same-sex relationships, drug users, or sex workers that get HIV, but people still associate HIV with behaviors. HIV is a disease, not a behavior. We wouldn't discriminate against someone with diabetes or high blood pressure.
Another false belief about HIV is that it's only transmitted through promiscuous sexual contact. Plenty of our patients have had one sexual encounter that infected them with HIV. It only takes one time to transmit it. Also, people falsely believe that HIV is a moral fault. For example, you got HIV because you did this or you got it because you are this. I really encourage everyone to think of HIV as an illness and not a behavior. Think about that person with HIV as a person who is just trying to stay healthy and manage their disease just like you would with diabetes or any other disease.
Workplace HIV Transmission
Workplace transmission is extremely rare. It’s even more rare in an educational setting. We'd never say it’s impossible, but I can't really think of a situation where it would happen an educational setting.
The CDC always talks about universal precautions, which have been around for a while. Universal means to use them with everyone. Notice they're not called HIV precautions or AIDS precautions, but universal precautions. This is because as we saw from those statistics before, not everyone knows that they're HIV positive. There could be someone walking down the street next to you who doesn't know they are HIV positive but they might be.
Universal precautions from the CDC include:
- Routinely use barriers such as gloves and/or goggles when anticipating contact with blood or body fluids. You might be in an elementary school and little Johnny is running and skins his knee and there's blood everywhere. As a general practice, you should be wearing gloves as you treat him. Not because you don’t know if he has HIV, but because it’s a universal precaution. Nobody needs to be handling anybody else's blood without gloves, especially in the workplace.
- Immediately wash hands and other skin surfaces after contact with blood or body fluids. Once you've taken off your gloves you should still wash up.
- Carefully handle and dispose of sharp instruments during and after use. This is something that is seen more in health care than in education but is important to know about. In the past, there was concern about needle sticks and needle stick infections because of exposed sharp needles. Now there are retractable needles so it’s not as much of a concern. The retractable needles allow you to give the injection or take the blood then push a button so the needle pops back up into the syringe, meaning there's no longer a sharp.
Forms of HIV Stigma and Discrimination
1. Self-stigma/internalized stigma
- Breakdown of self-confidence
- Fear of discrimination and lack of confidence to seek medical care and help
- Continues the cycle of silence and shame surrounding HIV
2. Governmental stigma
- A country’s discriminatory laws, rules, and policies regarding HIV
- Alienates and excludes PLHIV socially, educationally, and professionally
3. Healthcare discrimination
- Healthcare professionals can medically assist, provide essential information, and save lives of PLHIV.
- However, HIV-related discrimination in healthcare remains an issue.
- Delay or denial of treatment
- Isolating PLHIV from other patients
- Minimize contact with patients
- Violation of patient privacy and confidentiality
4. Employment stigma
- Termination or refusal of employment
- Discrimination from co-workers or employers
5. Community stigma
- Can force PLHIV to leave home and change daily activities.
- Family stigma and discrimination can lead to fear of losing shelter, custody, and ability to survive.
As you can see we're going back and forth from stigma to more of the science because I think that helps us to see the bigger picture. There are different kinds of stigma. I want you to think about HIV specifically when we talk about this.
Self-Stigma or Internalized Stigma
This is a breakdown of self-confidence where you might judge yourself, are concerned about yourself, or feel like you know you're nervous about your identity or if you have HIV. This might also cause a fear of discrimination and lack of confidence to seek medical health care and help.
As a health care provider, one of the big tragedies that I see is people who lack the confidence to seek medical care and help. I can think of many patients who said, “I thought I had HIV because I'd had unprotected sex or I've been using needles and sharing needles but I was so scared I would get judged from my doctor or a nurse or a secretary that I didn't go get medical care.” Those are people we see in the hospital bed with full-blown AIDS. We can give them medication to help get them better, but that doesn't have to happen.
Self-stigma continues the cycle of silence and shame surrounding HIV. For example, think about someone has internalized stigma and doesn't want to go get health care and doesn't get health care. Maybe that person gets really sick and doesn’t want to go on with life. That person might pass HIV on to someone else. That's a cycle of silence, shame, and HIV.
Governmental Stigma
Governmental stigma includes a country's discriminatory laws, rules, and policies regarding HIV. Even in 2019, there are still discriminatory laws, rules, and policies in different countries regarding HIV. This can eliminate and exclude people living with HIV socially, educationally, and professionally. It can stop them from getting an education, from being part of society, from professional advancement, or from getting a job.
Healthcare Discrimination
Health care professionals can medically assist, provide essential information, and save the lives of people living with HIV. However, HIV-related discrimination in health care remains an issue. This can include delay or denial of treatment, isolating people with HIV from other patients, minimizing contact with patients, and a violation of patient privacy and confidentiality. I’m going to share a couple of stories with you.
I have a research group at Emory that focuses on HIV, chronic pain, and opioids. One of the students in my research group came to me and was so upset. She is a 23-year-old very healthy young lady. She had gone to the dentist and said the dentist was asking about what she was studying. When she told him about her research and how she was excited about the research group he took his hands out of her mouth and said, “Why would you do that? Aren’t you afraid you’re going to get AIDS?” She said, “No because A it’s just research and B even if it was working with patients I wouldn't be at a risk for getting HIV.” She said she was educating him about how she wasn’t at risk and even if she was working with patients there's nothing she'd be doing with physical therapy to be at risk. She said to me, “I felt so vulnerable when he took his hands out of my mouth. I was not HIV positive, but I was laying in the chair mouth wide open and he’s pulled his hands away from me like I had the plague.” She didn’t have HIV, but there was that gut instinct from her dentist. We talked about it and she decided that she would no longer be going to that dentist. This happened in 2016 and it really has stuck with me because even in this day and age, even in a modern urban city like Atlanta with all the comforts of home and all the excellent medical facilities around, there is still that stigma. Plenty of patients are concerned about situations like this, especially if they are in an area where it's very rural or the doctor in their town wasn't as educated about HIV.
I have a patient who lived here in Atlanta and needed to go to rural Mississippi to attend to an ill parent. While he was there, he ran out of medication and had to have his doctor from Atlanta call in his medications at the pharmacy in this small rural town in Mississippi. The pharmacist would not fill the medication, said they didn’t have it, and he'd never heard of it. My patient went back and forth between his doctor in Atlanta and the pharmacy trying to get the pharmacist to order it, but the pharmacist refused and said he wasn’t going to fill it. He had to stay in Mississippi for about six months to tend to his ill parent. The entire time he was off his medications. When he finally made it back to Atlanta he was on his death bed, admitted to the hospital, and we almost lost him to AIDS. We were able to get him back on his medication and stable and I'm happy to say he's now healthy and thriving as we speak. This happened in 2017 and is an example of delay or denial of treatment. In addition, he said that because the pharmacist was so loud and made such a big deal about it, now everyone in the town knew that he had HIV. This is an example of violating patient privacy and confidentiality.
I'm giving you these examples not to be doom and gloom but to keep it real that discrimination is still going on.
Employment Stigma
Let's talk about employment stigma. This includes termination or refusal of employment. Unfortunately, you can look at a lot of non-discrimination policies and they don't have HIV listed. Another piece of employment stigma is discrimination from co-workers or employees. Unfortunately, we can't stop people from discriminating or from making discriminatory thoughts.
Community Stigma
Community stigma can force people living with HIV to leave home and to change their daily activities. Family stigma and discrimination can lead to fear of losing their shelter, custody, and ability to survive. If you'll remember I talked about a patient who disclosed her HIV status to her husband and was pretty much kicked out of the house. She lost her shelter. She had kids and was terrified about losing her kids and her ability to survive. That happened long ago, she didn’t lose her kids, and she's doing okay now. Unfortunately, there’s still a lot of stigma around HIV.
Effects of HIV/AIDS-Related Stigma
We talked about how discrimination can lead to HIV. In addition, HIV-related stigma can lead to discrimination. This occurs when people living with HIV are prohibited from or shamed when using healthcare facilities, in educational settings, or seeking employment. Stigma is the attitude and discrimination is the behavior. This may be because someone has stigmatizing beliefs about HIV.
Stigma blocks access to HIV testing and services, which makes transmission more likely. In general, if you have a lot of internalized stigma and anxiety about having HIV are you really going to walk into an HIV clinic or go to your primary care physician and get tested? Probably not.
Again, the more we can do to reduce stigma the healthier the whole world will be. It's in everyone's best interest to end stigma, both people with HIV and everyone else. It breaks my heart to think about people not getting health care or not being able to continue with their health care because of stigma.
Reducing Stigma By Being Educated About HIV
Let's shift gears a little bit and talk about reducing stigma. What's our part? Even if we're not doctors or we're not working directly with people with HIV, what can we do and what's our role to reduce stigma? Let's talk about words first, because words can make a big difference.
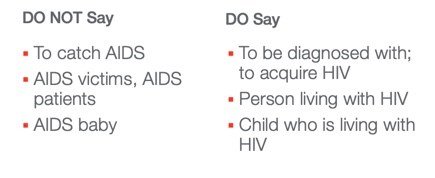
Figure 2. What to say and what not to say.
Do not say to catch AIDS. You don't catch AIDS. We talked about how HIV can be transmitted and it can turn into AIDS if it's untreated. Do not say AIDS victims or AIDS patients. It's important to devictimize people with AIDS. Do not say AIDS baby. I've heard people talking about an AIDS baby just like people used to talk about crack babies. A baby that is born with HIV is not born with AIDS. Babies can be born with HIV, but not AIDS. Let's say you get a baby in your program who was born HIV-positive. You know this because you know there are certain medications they have to get. You wouldn't refer to that child as an AIDS baby just like you wouldn't refer to a child with diabetes as a diabetes kid. It’s something that you live with and you don’t die from. Instead of to catch AIDS you should say to be diagnosed with or to acquire HIV. Instead of saying, “She caught AIDS last year,” you would say, “She was diagnosed with HIV last year.” You should say people living with HIV, a person living with HIV, or a child who is living with HIV instead of HIV baby.
Ending HIV Stigma and Discrimination
Again, what can we do to end HIV stigma and discrimination? One way is through the use of specific government programs that emphasize the rights of people living with HIV. When aware of their rights, people living with HIV can be empowered to seek care and to take action if their rights are violated. Make changes in institutional policies, at community levels, and individual personal levels. Now, let's be more specific about what you can do as educators.
Reducing HIV Discrimination in Schools: What Can YOU do?
- Institutional Level:
- Does the school/institution have policies against HIV-related discrimination?
- Are mechanisms in place to report, document, and address cases of discrimination against PLHIV?
- Are teachers/daycare workers receiving training:
- On non-discrimination and non-stigma in the context of HIV?
- About serving the diverse needs of students and families?
- About their own HIV-related stigma to better understand and combat it?
- Are there ongoing education and skills-building for staff?
Reducing HIV discrimination in schools. What can you do in an institutional or school level? One question to ask is does the school or institution have policies against HIV-related discrimination? To find out, look in your non-discrimination policy and see if it is specific to HIV or if not HIV, is it specific to health issues or health. You might see wording such as, “… do not discriminate on the basis of race, sex/gender, sexual orientation, or health status.”
Another question to ask is are mechanisms in place to report, document, and address cases of discrimination against people living with HIV. If you found out that a colleague or a student was being discriminated against because of HIV status what could you do? What could they do? What are their resources?
Are teachers and daycare workers receiving training on non-discrimination and non-stigma in the context of HIV or about serving the diverse needs of students and families? Are they receiving training about their own HIV-related stigma to better understand and combat it? I am a huge fan of staff trainings. I think that they can be really helpful on so many levels.
You might have a staff training about what is HIV, what is stigma, and how can we work to decrease it, eliminate it, or just prevent it. Families have diverse needs and you can look at that in a global sense or specifically on a child that may have HIV.
Self-reflection is always hard. It's difficult to look at what are our own stigmas. What do you think of if you close your eyes and think of AIDS or HIV? What comes to mind? If you think about how people get it, what comes to mind? Is there a part of your brain that says, “Well you know it's when people do this or people choose to do this or people behave like this.” It’s hard and it takes a lot of work to face our own stigmas, but the better we face it and understand it, the better we can combat it.
Are there ongoing education and skills-building for staff? One time is not usually enough. At one training you might learn about non-discrimination and non-stigma and HIV. At the next one, you might learn about some ways to serve the needs of people living with HIV, whether it’s children or parents who are HIV positive. You might have a separate skill-building session where you self-reflect on what your own stigmas are.
There are plenty of assessment tools about self-stigma online. You can just do an internet search for HIV stigma quiz. In our department, everyone was told to bring their laptop to the staff meeting to complete a quiz. Our director said, “I will not look at these results and I will not ever have access to them. But I want you to see what your stigmas are and I want you to see what your prejudices might be internally.” It was a really good experience because no one felt like they had to answer the questions a certain way because someone was going to see it. That allowed people to be really honest. We were the only ones who saw our score and what stigmas and prejudices, or implicit biases, we had. These biases we have aren't explicit. We're not shouting out discriminatory things and saying, “I don't like you. I'm not going to hire you or work next to you because of this.” They are internal things. I would recommend that if you are having some kind of staff training about your own HIV-related stigmas to include an activity like this so people could do it on their own and reflect.
Reducing Stigma
- Policy level:
- Be familiar with your institution, state, and federal anti-discrimination policies and confidentiality laws
- Community level:
- Collaboration between organizations to better serve students/youth
- Identify community partners such as AIDS service organizations (https://locator.aids.gov/)
- Consult with local pediatricians as needed
- Know your community resources
- There are many stigma-reduction interventions implemented by health departments and community programs: engage your institution!
How can we reduce stigma at both a policy and a community level? At a policy level, be familiar with your institution's, state, and federal anti-discrimination policies and confidentiality laws. Every organization should have them. They may not all talk about HIV and AIDS, but be familiar with what your institution does say. It should at least say they do not discriminate based on health status. HIV is a health diagnosis so that legally should be covered. What are your state laws about protection for HIV status? What are federal anti-discrimination policies and confidentiality laws about HIV?
The community level is where I always say, “This is where the rubber meets the road.” We are all part of some community somewhere. Think about what collaborations are there already between organizations to better serve students and families. When I talked about staff training some of you may have felt as if you didn’t know how to do that or that you didn’t know anyone in your organization who knows how to do that. Community partners will be your best friends. No matter where you are there will likely be an AIDS service organization somewhere for that area. Go to http://locator.aids.gov/ to find an AIDS service organization near you. This site is a governmental organization and is updated all the time. Consult with local pediatricians as needed if you have even one child who has HIV and you're not exactly sure of the best ways that you can make sure you are serving this child's needs best. Local pediatricians will be happy to answer questions.
Know your community resources. There are so many stigma reduction interventions that are implemented by health departments and community programs and we really want to engage your institution. AIDS service organizations, health departments, and community programs are thrilled to have more and more people to partner with. If they can partner with your school or daycare center that would be wonderful.
- Interpersonal level
- Social support from peers
- Peer and family acceptance
- Education
- Teaching those connected with youth about HIV transmission, care, and testing is essential to reducing stigma
- Overcoming implicit bias
- Recognize your own implicit bias toward PLHIV
- Individual Level
- Encourage self-esteem and leadership among youth
- Encourage education about HIV transmission and prevention among youth
We talked about the different levels of people's worlds. We talked about policy, community, and now we’re getting smaller with interpersonal and individual levels. The interpersonal level is person-to-person. This includes social support from peers. Do they have social support or are they isolated and stigmatized? Is there peer and family acceptance? In some families with children who are HIV positive, the parents will keep it a secret. They don’t want the grandparents, aunts, or uncles to because of stigma. As I’ve been saying, the only way we can combat stigma is to normalize things. I always say that to my patients and when talking about HIV, the more we normalize things the less stigma there will be.
Teaching those connected with youth about HIV transmission care and testing is essential to reducing stigma. Stigma is about fear. Fear is lack of knowing things. We're scared of things we don't know. Kids are really scared before the first day of school. They don't know what's going to happen, what their teacher is going to be like, are their friends going to be in their class, or what are they going to learn. We're scared of things we don't, whether we are a child or an adult. We need to educate ourselves and our communities.
Recognize your own implicit bias towards people living with HIV. You could even just Google implicit bias HIV and read up on it or take a quiz. However, just because you take a quiz doesn't mean that all of a sudden you don’t have bias anymore. Just recognize it. Maybe the quiz said something about how you think people with HIV have it because of their behavior. Take time to think about that and work on that bias.
At the individual level, encourage self-esteem and leadership among youth. This includes every youth, from toddlers up to age 18. Help them understand that they are an important individual. You want to keep yourself healthy and strong so you can have a bright future in front of you.
Encourage education about HIV transmission and prevention among youth. Schools and states have different laws about it. It should start early in school and in the home so we can protect our kids.
Reducing HIV Discrimination in Schools: What Can You DO?
- Attitudes and Behaviors Checklist
- Does the workplace hold stigmatizing attitudes/beliefs and exhibit stigmatizing behaviors and discrimination toward PLHIV?
- Do workers understand how children are infected with HIV?
- Do workers understand their own low personal risk for HIV transmission from students?
- Do workers understand universal precautions (i.e. wear gloves if you are cleaning body fluids!)
An attitudes and behaviors checklist is something I think can help reduce HIV discrimination. Think about these questions. Does the workplace hold stigmatizing attitudes and beliefs and exhibit stigmatizing behaviors and discrimination towards people living with HIV? I'm not talking about a poster up in the break room that says, “No HIV allowed.” I'm talking about what I call water cooler talk.
Do workers understand how children are infected with HIV? Do workers understand their own low personal risk for HIV transmission from students? Remember, stigma is based out of fear. We never say never, but there's an incredibly low personal risk for HIV transmission from students.
Do workers understand universal precautions? This includes wearing gloves if you're cleaning up body fluids. Everyone can use a refresher about that. I know I'm a broken record saying it over and over, but it’s so important to educate people because the more we know about HIV the less stigma will be a problem.
Scenarios…Let’s Discuss!
Let’s go through a couple of scenarios.
- You are a daycare provider and a child cuts his hand, bleeding slightly. Would you tend to the cut differently if you knew that the child did or did not have HIV?
Hopefully, the answer is no, you would not treat that child differently. We should use universal precautions. Even if the child did have HIV, was bleeding profusely from the hand, and you picked it up in your bare hand unless you had a massive gaping wound on your own hand, it's pretty unlikely that you'd be infected. Use universal precautions and treat everyone the same.
- In the break room of your elementary school, you overhear several colleagues saying that they would never want to work with a child with HIV, as they would fear getting infected. What would you do?
If you feel like you can do it say, “Do you know how HIV is transmitted?” Or, in a conversational way you can say, “It's just transmitted in these certain ways. It's almost impossible to get infected with HIV just by being a child's teacher. There is really no reason to fear because children get infected through their pregnant parents. So, there's really no risks to you personally or very low risks to you personally.” Remember, these stigmas are based in fear and the more we can do to educate and decrease the fear the better.
As I end, I want to remind you that stigma does still exist. People are still being infected with HIV daily. What we can do as educators and as citizens is to educate ourselves and others. All children deserve a bright future and as educators, we have an immense responsibility and an immense privilege that we can be at the forefront of this. Whether that's helping to educate people in the break room over the water cooler or supporting children and their families who may be affected by HIV that as educators, especially of young children, we have a great responsibility and a privilege to be able to ensure that all children have a bright future.
References
http://aidsinfo.nih.gov/education-materials/fact-sheets/19/45/hiv-aids--the-basics
https://www.cdc.gov/hiv/group/gender/pregnantwomen/index.html
https://www.avert.org/professionals/hiv-social-issues/stigma-discrimination
http://www.unaids.org/sites/default/files/media_asset/2014unaidsguidancenote_stigma_en.pdf
https://www.cdc.gov/hiv/workplace/healthcareworkers.html
Resources
https://www.avert.org/professionals/hiv-social-issues/stigma-discrimination
Citation
Pullen, S. (2019). Reducing the Stigma of HIV/AIDS. continued.com - Early Childhood Education, Article 23260. Retrieved from www.continued.com/early-childhood-education
