Editor’s note: This text-based course is an edited transcript of the webinar, Seizures and Seizure Management in Early Childhood, presented by Nancy Nathenson, RRT.
Learning Outcomes
After this course, participants will be able to:
- Define seizures and epilepsy.
- Identify the correct and incorrect steps for helping a child having a seizure.
- Recognize when it would be necessary to call emergency personnel (911) in the event of a seizure.
Introduction and Definitions
I speak with a little bit of experience because my husband has a seizure disorder. Although I don't care for a child with a seizure disorder, I may interject some of the experiences that I've had with him. I am also seizure recognition and first aid certified by the Epilepsy Foundation of America. We'll talk more about the Epilepsy Foundation and all that they can do for you. Because a majority of our audience is in the United States, I will refer to 911 as the number to get help when needed. 911 services in the United States were started about 50 years ago, and cover the United States, North America, and other US territories. However, for our international audience, please ensure you're aware of the emergency number in your area to call for help. For example, in the European Union and India, the number is 112, and in Australia, 000. Please be mindful of that.
Let's define seizures and epilepsy. A seizure is a sudden uncontrolled electrical disturbance in the brain. It can cause changes in a person's behavior, movement, feelings, and levels of consciousness. It can impact all of those things or it can impact just one of those things. Every individual is different. According to the Mayo Clinic, epilepsy is having two or more seizures at least 24 hours apart that are not brought on by an identifiable cause. The reason for the seizure is unknown and they happen close together. A seizure occurs when there is a change in electrical signals in the brain. There's a short circuit in the way messages are sent to the body. Seizures can occur with other medical conditions as well, and not everyone that has a seizure has epilepsy.
Let's talk about the impact of seizures and epilepsy in the United States. One in 10 people will have a seizure in their lifetime. There are currently approximately 330 million people in the United States. About a million of them still have seizures even though they are on medication to prevent them. Luckily, my husband's seizures are controlled with medication. Nearly 3 million Americans of all ages live with epilepsy. Remember, epilepsy is a medical condition that happens when there are frequent seizures close together. One in 26 people will be diagnosed with epilepsy during their lifetime, and 25% of cases develop before the age of five. This is the demographic most of you work with. Males are more likely than females, and African Americans are more likely than Caucasians to have epilepsy. While this course is focused on what happens to a child during a seizure, the information is also applicable to others of any age. The terms individual, person, and child may be used interchangeably.
Seizures in Children
Let's talk about seizures specifically in children. About 3% of all children have seizures when they're less than 15 years of age. 50% of these are febrile seizures, meaning they occur when there is a fever. They are the most common type and can happen with an ear infection, chicken pox, or even the common cold. The risk factors for seizures in children include genetics, having something to do with the family medical history, and developmentally delayed children. One in four children that have febrile seizures will have another one within one year.
Children with seizures often have other disorders that accompany the seizures. One of those things is fainting. Fainting is when blood pressure drops and there is less pressure or circulation to the brain. The most common reason fainting occurs is dehydration. If this happens to a child, the doctor may say the child needs to drink more water because the more volume of water you drink, the more blood you've got circulating. It is also important to eat on time and to eat salty foods because salty foods help you to retain water and keep that volume in your bloodstream.
Another common disorder seen with seizures is breath-holding. Breath-holding spells can happen in children from six months to six years of age, but mostly they happen in children that are six months to 18 months old. Breath-holding usually occurs after the child has been very angry or if they are frustrated, startled, or when in pain. A child may even pass out for a minute or two when they do their breath-holding. Cyanotic breath-holding, which means the face of the child turns blue from lack of oxygen, usually occurs after a child cries really hard, often from anger or frustration. Pallid breath-holding is when the face turns white from being startled or in pain. It is important to note that children do not have breathing spells on purpose. They don't have control over this.
Night terrors can affect toddlers and preschoolers during their deepest stage of sleep. They can last for a very short time and the child can recover and go right back to sleep and be fine, or they can last up to about 45 minutes. Children have migraines just like adults, but they generally don't last as long as migraines in adults do. Migraines can be genetic and you can have just a history of migraines in the family or certain foods and beverages can cause migraines. Sugar and some carbohydrates really affect the brain. Migraines can also happen from stress, anxiety, infection, or even minor head trauma. You might see a child with seizures who also has psychic disturbances, severe anxiety, or strong fear.
Risks Related to Seizures
There are risks related to seizures. Physical injury can occur when someone's having a seizure and are not able to control their body. One time my husband was driving a car and he had a seizure. Another time I was with him and he had a breakthrough seizure. I had to help him guide the car off the highway and put on the brake. That was a very scary situation. Sometimes people having seizures have difficulty breathing. Other seizure emergencies and even early death can occur, such as accidents or drowning. If a child has breathing or heart problems and they have a seizure, that could cause early death. There is a risk of suicide in people with epilepsy, sometimes because of the type of medication that they're taking and the high level of this medication in their bloodstream. Some medications, such as pregabalin or Lyrica, can cause suicidal thoughts, hallucinations, and depression. Sudden unexpected death (SUDEP) may occur, although it's rare. One in 1000 individuals with epilepsy that have uncontrolled epilepsy can die from SUDEP. That happens most often when they have uncontrolled seizures, when they have seizures at night, or when they have violent tonic-clonic seizures. We will talk more about tonic-clonic in a minute, but that's just when your body is stiff and shaking terribly.
Did you know that most seizures are not medical emergencies? That's a relief. A person may not be even aware that they are having a seizure. Seizures are not contagious. A person cannot swallow their tongue during a seizure. It's been a misconception over the years that you put something in the mouth to keep the individual from swallowing their tongue, but that cannot happen. Epilepsy, as I mentioned, is a medical disease. Sometimes a person can die from a seizure.
Seizure signs and symptoms of seizures vary from person to person. It's all individual and is not the same in every person. However, in most cases, they are usually consistent, look the same, and are predictable for each individual. You get used to a person and the type of seizure that they have and when they might occur. Anything the brain can do normally the brain can do during a seizure. During a seizure, you may move, see, feel, hear, smell, or do other things even if you don't want to while you're having a seizure. Also, the heart will keep beating and the lungs will keep breathing in nearly every case.
Characteristics of a Seizure
In general, seizures can result in changes in body or facial movement. It can also cause changes in sensations, such as the sensations a person might feel inside their body or just on the outside of their body, such as their skin. Behavior can change when there's a seizure. Someone may be fine and then they might be very violent or be misbehaving. A person's speech also can be affected. The person may not be able to speak during a seizure, or you may not be able to understand their speech during a seizure. Awareness also can be affected so they can be totally aware of their surroundings or not aware. The area of the brain involved determines what the seizure looks like, and we'll talk more about that now.
Types of Seizures
The type of seizure depends on where it starts in the brain. Focal seizures occur in a specific spot in the brain. If it's occurring in the speech center of the brain then it will affect the individual's speech. When generalized seizures occur the disruption and electrical activity are all over the brain. It's not centralized so they could have speech and motor disruptions, as well as behavioral disruptions. Seizures can occur whether or not awareness is affected and may or may not involve other symptoms such as movement.
General Symptoms/Warning Signs of a Seizure
Here are some general symptoms of seizures to look for if you're watching children. They may be staring or look like they're daydreaming. They might not respond to words or noises for brief periods, or if you're chatting with them and they're not responding, rapid eye blinking with staring can occur. They may appear confused or in a daze. They might nod their head rhythmically when they're not aware or conscious. Their body could just stiffen all of a sudden or they could fall suddenly for no apparent reason. Loss of consciousness and loss of bowel or bladder control can also indicate that there is a seizure going on.
Infantile Spasms
Infantile spasms are quite common in children less than 18 months old. They may be associated with intellectual disabilities in a child, but not always. During an infantile spasm, there are sudden, repeated uncontrolled movements by the child. They will have a flexed stature, so their body will be flexed and they may bob their head or scrunch up their little body. When this type of thing occurs, it often occurs on awakening. If you're caring for a child and they're awakening from their nap, be observant of that. If you see the signs, take a video of it and then offer that information to the parent, or if you're a parent of a child yourself take it to the physician and obtain a diagnosis if it's infantile spasms. Then they can prioritize the treatment that the child might need. Infantile Spasm Awareness Month happens every December because this is something that's common.
Febrile Seizures
I mentioned febrile seizures earlier. These occur in children between six months and six years of age. It is the most common type of seizure in children. They're more likely caused by viral infections, which can't be treated by an antibiotic, and less common bacterial infections, which can be treated by an antibiotic. For example, the flu virus and the virus that causes roseola commonly have high fevers which appear to be frequently associated with febrile seizures. Roseola is when a child gets a rash all over them and they run a particularly high fever. Other things that may cause high fevers are brain infections, outside temperature, and infectious agents being breathed in. There are many different things that can trigger febrile seizures. Most children with febrile seizures rarely develop long-term health problems. There is possibly a genetic cause of febrile seizures. Febrile seizures have no negative effects on behavior, scholastic performance, or cognition. Most febrile seizures are very short and they self-terminate, or, stop on their own. Most don't require any type of long-term treatment with anti-epileptic drugs.
Seizure with No Change in Awareness
Seizures that occur with no change in awareness are focal aware seizures. The individual is fully awake and aware during the seizure. They generally last about one to three minutes. There can be any change in behavior with this type of seizure, such as motor, sensory, or psychic. A motor change in behavior might be a rhythmic twitching of the body or jerking of the face and the arms and legs. A sensory change could include tingling, sounds, smelling something specific, or visual changes. Psychic changes are changes in thinking, feeling, or perceptions, so they could become terribly fearful or anxious or have that feeling of deja vu as if this just happened before. These seizures with no change in awareness are often just called focal seizures.
Seizure with Confusion or Not Aware
Seizures with confusion or they are not aware are called focal impaired awareness seizures. The person is not aware of what is going on or is confused. They may have a blank, dazed state. They're relatively short-lived and generally last about one to three minutes. The child may have some repeated purposeless movements called automatisms, such as lip-smacking, chewing, or clapping their hands. They might have clumsy movements when they're confused and not aware during this type of seizure. They may not be able to talk. Many seizures are often followed by side effects for a while, such as tiredness, headache, or nausea. The child could become combative if they're restrained. We will talk more about how it's best not to restrain an individual with seizures.
Generalized Seizure Terms
Remember, a generalized seizure is one that affects many parts of the brain at once and can affect muscle tone or tension. Here are some terms that are important to know. Tonic means muscle tone. Stiffness may occur and the individual could just fall over like a tree trunk. Atonic means an absence of tone, which means that the body could be very loose or floppy. They may fall like rag dolls and may have the twitching and jerking of muscles in an atonic seizure. Myo means muscle and clonic means jerking, so myoclonic means brief jerks in a muscle or a group of muscles. The arm may begin to jerk and then as the seizure progresses, that jerking will move throughout the body so it'll move to the next arm or the legs, et cetera. Clonic means rhythmic jerking in part or all of the body.
Seizure with Loss of Consciousness
Seizures with loss of consciousness mean the individual has passed out. During tonic-clonic seizures the body is in a very flexed stature with tense muscles and jerking. If a child is having a tonic-clonic seizure you might hear the child cry out with a sudden hoarse-sounding cry. They'll lose consciousness and may fall because they have stiff arms and legs (tonic) and then rhythmic jerking (clonic). They may have shallow breathing and drooling may occur. They typically last between one and three minutes, and the child could have a loss of bowel or bladder control with this type of seizure as they lose consciousness.
Seizure with Staring and Not Aware
When someone has a generalized absence seizure they usually stare and are unaware of their surroundings. A pause in activity occurs with a blank stare and they have a brief lapse in awareness. They might have a chewing or blinking motion during this seizure. It may occur many times a day, but it lasts less than 20 seconds. After the seizure, the child will return to normal immediately. These are very short-lived seizures and the person is totally fine after and not aware that they happened. These seizures are often followed by a headache and confusion, even though they seem back to normal. They might be tired or sore, especially if they bit their tongue when they were doing the chewing motions. They may have some speech difficulty after.
What to Look for During a Seizure
Early Signs
What do you see or hear first? That's important to note. Was the person able to tell you they didn't feel well? Some individuals have an aura or feeling hours or even days before a seizure occurs so they can ensure they are in a safe place and they take their medications on time, et cetera. This happens more in adults than children. It is called a prodrome and is considered part of the seizure. There's a change that occurs in the brain that precedes a seizure. If my husband ever has a breakthrough seizure, he has this sense of impending doom or a sense of feeling dread just before the seizure. The child could have intense joy or fear, it could be like a wave going through their brain, or a sensation in their stomach. They may feel a tiny bit weird in their tummy and have tingling in the body, or they might have an unusual taste in their mouth or smell. These are examples of aura, which is a tip-off to a seizure.
During Seizure
During a seizure, you need to note what happened next. Was the person awake, confused, or not conscious? What part of the face and body was involved? Did you notice any changes in speech or behavior during the seizure? What about after the seizure? How long did it last? Did the person quickly return to normal? Was the person tired or confused or having other symptoms?
After Seizure
What do you expect after a seizure? The recovery period after seizures is called the postictal period. That's the time immediately after a seizure, just before the child returns to their usual state of awareness and function. How a person feels and functions is going to depend on what type of seizure was experienced. If it was a very simple seizure just involving not being aware for a while the person will have fewer effects than if it was muscle jerking, facial involved seizure. After a seizure, help the child to a safe place to rest. Check and see if they're alert and aware. Even if they seem back to normal, give them time to come around and make sure that they're not confused. Stay with them until another adult arrives.
Seizure First Aid
There are three basic principles of seizure first aid for any seizure. Stay, safe, and side. These are the Epilepsy Foundation recommendations. Stay until the individual or the child is awake and alert. Safe, keep them away from harm. Time the seizure. Check for a medical ID to see if they have epileptic or seizures on a bracelet. Keep their airway clear. If individuals bite their tongue they could have bleeding in their mouth or they might be drooling during the seizure. Loosen tight clothing, especially anything that's constricting their breathing. Place something small and soft under their head. To recap, stay with them, keep them safe, and turn them on their side if they are unconscious or not aware. Other interventions include putting something behind their head and making sure that the clothing is loosened.
Figure 1 shows an excellent poster that is downloadable from the Epilepsy Foundation. There is a link to this poster in the resources section at the end of this course. This is great to post at your facility, store in a notebook, nearby in the car, or give to families and caregivers. It is important to look for a medical bracelet when a child is having a seizure.

Figure 1. Seizure first aid poster from the Epilepsy Foundation.
What NOT to Do
There are some things you should not do during a seizure. Do not restrain or forcibly hold the person down. Restraining someone during a seizure does not stop the seizure and will not make things better. It can lead to injury or make the person even more confused, agitated, or even aggressive. They're not fighting on purpose, please remember that. If they try to walk around, just guide them away from the street or guide them away from harm to some kind of enclosed safe area. Just gently keep them safe if they insist on walking around.
Do not put anything in their mouth. Remember, they cannot swallow their tongue and it's not appropriate. Do not give food or water until the person is awake and able to swallow. Rescue medications that are in the treatment plan for the child can be given, but that is usually a small pill that's put in the cheek, a nasal spray, or medication to be given up the rectum. If you try to give food or water to an individual during a seizure they may not be fully awake and aware and when swallowing, it may get into their lungs. That will cause a whole different set of problems.
Seizure Action Plan
Figure 2 shows part of a Seizure Action Plan from the Epilepsy Foundation that can also be downloaded from their website. When completed, this document provides you with very important information including the emergency contact for the child, what type of seizure the child has, how long they last, how often they occur, and what happens. It provides specific instructions on what to do, when to call the provider, and when to call 911 emergency services. It also includes when rescue therapy may be needed and what type of rescue therapy medications the individual would need. This would be in addition to the regular medications that they might take all the time. The second page of the Seizure Action Plan has things to do for the child after the seizure, any special instructions, what medicine they are on regularly, and all of the health care contacts.
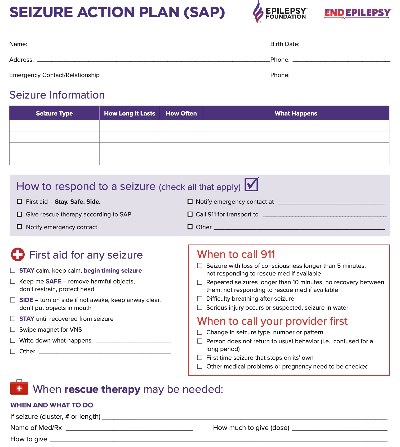
Figure 2. Sample Seizure Action Plan from the Epilepsy Foundation.
When Seizures Happen
Any time someone has a seizure and there are people around they want to help, but they are also curious and just want to see what's going on. Let's talk about what to do when seizures happen in various settings. You want to try to keep space around the child and make sure that people are not crowding the child. People want to help, so you may elicit someone's help by asking them to help move people aside, make a path for emergency services, or if you know the parent is coming you might need someone to go and open the door for them. You might have someone direct emergency personnel to an elevator or have someone outside watching for emergency services. Also, a person standing around could offer something to put behind the child's head.
Setting: Wheelchair
If a seizure happens while someone is in a wheelchair, keep the person in the wheelchair if possible. Secure the wheelchair, make sure the brakes are on, someone's holding onto it, and fasten the seatbelt loosely if it's not fastened to prevent the person from falling out. Protect and support the head because whether it's a wheelchair or a stroller, the child could be throwing their head around and it could be knocking into the bars of the stroller or maybe the wheelchair. Make sure that breathing is not blocked and saliva can flow from the mouth. That may mean that you gently curve the mouth over so that drooling can occur and flow out of the mouth. If there's a Seizure Action Plan, follow that action plan.
Setting: At the Bus Stop or On the Bus
If you are at a bus stop you might see a child kind of in a daze and maybe walking into the street or off the curb. Hold them back gently, call for help, and keep them out of the street. Don't leave them alone. Follow the other seizure actions we've discussed. If a seizure happens on a school bus with loss of consciousness, make sure you place the child on their side facing away from the seat if they're in the seat or away from the seat back so they have more openness. You can also lay them down in the aisle. Again keep people away so they aren't startled when they do wake up. Remain with the child until they're awake and alert, and call 911 if necessary.
Setting: In the Water or When Swimming
If someone is in the water or swimming and a seizure occurs, support the head so that the mouth and nose are above water. The child should be removed from the water as soon as can be done safely. Give seizure first aid, remembering all the first aid steps. If the child isn't breathing, begin rescue breathing. Rescue breathing is part of CPR. In CPR you do chest compressions, but you do rescue breathing when the heart is still beating and an individual needs just help with their breathing. Always call 911 even if they have fully recovered. If it happens in water, 911 is called.
Calling for Emergency Services (911)
When to call 911
When do we call for emergency services? Call 911 if a seizure lasts longer than five minutes or if there are repeated seizures, for example, if a seizure occurs, the child recovers, and then has another seizure. If there is difficulty breathing call 911. Sometimes they're still breathing and their color looks good, but if you see that they are having difficulty breathing and trying hard to breathe then call 911. As I mentioned, if the seizure occurs in the water call 911. If the child is injured when they have a seizure, or they're sick call 911. If the child does not return to their usual state or if it is a first-time seizure are additional reasons to call 911. Remember to follow the Seizure Action Plan if you have one of those on file.
Share What Happened During the Seizure
You might need to share this information with a parent, caregiver, or emergency personnel. When a seizure occurs, you might assign someone to take notes or jot down what you're observing. How long did it last? What did you observe? Was the person injured? When and where did the seizure take place? Did the person take or were they given any medicine? That's important for a parent or especially emergency services to know. Was the seizure different from anything usual that you would know about the child? You might want to gather information from people that know the kid better than you do. Provide written notes if possible.
Caring for a Child with Seizures
When taking seizure medication, it's important that the medication is taken on time. It's also important to monitor for side effects and changes in behavior when a child starts on medication. Ensure adequate sleep and a healthy diet. When we get good sleep, our brains reset and our stress hormones level out. Good sleep is a time when our body naturally heals itself and gets prepared for the day ahead. Have a support system. Make sure that your family, friends, teachers, caregivers, and coaches know what's happening with the child. These people, along with your health care support system will help you care for the child. Keep the child active. The child needs to be able to play safely in all areas. Monitor how the child is coping. Some kids cope really well with this chronic type of condition and others not so well, so be very mindful of that. Keep a seizure diary of when they happen, how long they occur, and all of the details. This is true for kids with allergies as well. You want to keep a good diary of when the child has any kind of reaction to something that they're allergic to or some type of food.
Epilepsy
The Epilepsy Foundation has a wealth of information online for many different individuals including those caring for children of all ages in school or child care. Their mission is to lead the fight to overcome the challenges of living with epilepsy to accelerate the therapies to stop seizures, find cures, and save lives.
Epilepsy is a neurological disease that causes individuals to have recurrent unprovoked seizures, meaning we don't know what has caused them. Thirty percent of the children that are diagnosed continue to have repeated seizures into adulthood. The good news is that 70% of children that are diagnosed with epilepsy can improve over time. Their little brains grow, develop, and mature and things can get better. If epilepsy starts before age 18 it is considered a developmental disability. Anytime you have a seizure and if you have recurrent seizures, it affects the brain. Depending on where it occurs, such as the speech center, memory center, or learning center, it can cause developmental disabilities.
Statistics
Here are some statistics about epilepsy. Worldwide, 65 million people have epilepsy. That includes 3.4 million people just in the US. There are 150,000 new cases diagnosed each year, with close to a half a million of those cases being children and youth in the United States. Epilepsy can affect anyone, it doesn't matter who you are. It's a syndrome associated with other health problems, so an individual may already have some cognitive or neurological problems or psychiatric problems such as mental illness. It also is associated with learning difficulties and psychological and social problems.
Common Causes
For many, the cause of epilepsy is unknown. In fact, only about half of individuals that are diagnosed with epilepsy know the cause. Knowing the cause can help the doctors and parents understand what is to be expected over time. Some of the reasons that epilepsy can occur are brain trauma, brain tumors, and brain infections. My husband had brain trauma because he had brain surgery to remove a brain tumor that was pushing on the area of his brain that controlled the left side of his body. He became paralyzed on the left side after the surgery to remove the tumor and after the trauma of the surgery. He's been on AEDs, or anti-epileptic drugs, for some time. Brain injury at birth can cause epilepsy This can include babies being born with a lack of oxygen or external forces like forceps, things like that put pressure on their tiny heads and their brain. There can be changes in brain development that cause epilepsy. Stroke can also cause epilepsy. One in every 4,000 newborn births has a stroke. A stroke is among the top 10 causes of death in children. Genetics, including a history of epilepsy in the family, is another cause.
Types
Here is a selection of types of epilepsy, including some common ones.
- Temporal epilepsy occurs in the temporal lobes of the brain responsible for learning and memory. The temporal lobes are located on your temples between your ears and eyes.
- Intractable epilepsy is when a person's seizures fail to come under control with treatment.
- Reflex epilepsy is when specific triggers bring on seizures, such as cold temperatures, stress, or other things.
- Psychomotor epilepsy is typically limited to the temporal lobe of the brain and results in impairments of responsiveness and being aware of one's surroundings.
- Photosensitive epilepsy is when seizures are triggered by flashing lights or contrasting light and dark patterns. Sometimes you'll see this on video games, movies, or television shows and they'll give you an alert to let you know that there could be lights and distractors on the TV that could cause a seizure.
- Post-traumatic epilepsy is a recurrent disorder resulting from injury to the brain, such as surgery, concussions, and things of that nature.
Diagnosis
A medical professional or neurologist diagnoses epilepsy. There's no specific test to test for epilepsy, but the doctor will get blood tests to get a baseline of the chemistry of the blood in your body. They'll also do blood tests to check for liver, kidney function, and diabetes, which can be the cause of seizures. That will help them drill down and see what's happening. Imaging tests like X-rays can be used to see if there's anything that can be physically seen in the brain. An EEG, or electroencephalogram, is brain wave testing done with little electrodes taped to your skull that records all the busy electrical brain waves. Some of the most vital information we'll get from parents or individuals who experience seizures includes the patient and family medical history, as well as all of the details of what happens during a seizure.
Status Epilepticus
Status epilepticus is a seizure that won't stop after several minutes. This is a real crisis. It could be a seizure greater than 30 minutes or repeated, shorter seizures without a return to normal. These are most common in children less than two years of age with a history of tonic-clonic seizures, which are the ones with stiffness and jerking. Suspicion of a status epileptic event occuring requires emergency 911 response right away.
Treatments
There are three goals of epilepsy treatment. First, we want to achieve complete seizure control. We know that that doesn't occur in everyone, but that is our goal. The second goal is preserving the quality of life. Anytime you have this type of disorder, it affects not only the individual but the family and the direct caregivers as well. The third goal is to avoid any adverse effects, such as side effects from the medication or any adverse events where the individual would not find themselves not to be safe, get injured, and so forth.
Treatment usually begins with anti-epileptic drugs, commonly called AEDs. Other treatments include epilepsy surgery, which is brain surgery, implanted stimulation devices, medically prescribed diets, and complementary and alternative medicine. Complementary interventions or medicine refers to practices that are out of the mainstream. This does not include medical or biomedical interventions like medication, surgery, or things like that. They are often used to complement, in other words, in conjunction with, medical treatments. Examples of complementary and alternative medicine include massage, aromatherapy, mindfulness meditation, herbal remedies, and vitamins. Vitamins aren't considered biomedical treatments. In a complementary intervention, people might take vitamin E, vitamin D, B6, magnesium, and folic acid. Alternative medicine is when these types of interventions or treatments are used instead of biomedical.
Anti-Epileptic Drugs (AEDs)
Anti-epileptic drugs, or AEDs, were introduced in 1857. Anti-seizure drugs alone control seizures in only about two out of three people. There are a wide number of drugs to treat epilepsy in children. In fact, nine new medications have become available just in the last decade. That doesn't mean that the newest drug is the best. There's no miracle cure for epilepsy. However, doctors are getting better and better at fine-tuning treatments based on the use of newer and older drugs.
When you take an anti-epileptic drug, your drug level must be monitored, so blood tests are done to check the level. There is a therapeutic range of how much medicine should be in the blood to protect that individual from seizures. Urine tests are performed to see how the body is reacting to the medicine that's being used. It is important to watch for side effects as they are wide-ranging. They don't always happen, but there are different ones for different drugs. Some of the side effects include fatigue, dizziness, nausea, vision changes, and rashes. My husband had a severe reaction to Dilantin when they gave it to him for his uncontrolled seizures, and he would swell up and be red all over like a lobster. Other side effects include gait disturbances, which are disruptions in how you walk, behavior changes, and mood changes. When these types of drugs are used, they are started at a very low dose and slowly increased. It may take weeks or months to adjust to these medications. You have to figure out what type of side effects you can tolerate for that period until you get to that sweet spot. More than one medication may be needed.
Seizure Triggers
It's important to identify when a child has a seizure if there's a particular trigger. Some triggers are caused by just missing seizure medication or stopping it suddenly. Also, not getting enough or good sleep, stress, or being sick with another illness or fever may trigger seizures in an individual that's controlled. If someone is photosensitive, flashing lights can also be a seizure trigger.
Seizure Control
We want to understand the details of a child's medicine. It's very important to know what to take, how to take them, how often, when, and why are you taking them. The more children know about their seizure disorder and their medication, the better. We want to empower our children to understand what's happening. You need to follow specific instructions, so for example, if it says to take it with food or take it just with water, follow that instruction. Have a specific time set up to take medication so that it's easy to remember. That could be before meals, at breakfast, and at dinner, or maybe it's at bedtime. Make sure you get those blood tests checked by your health care provider. Also, track if the medicines are working, so as you monitor the child you can see how they're adjusting.
When More Help is Needed
When is more help needed from just taking the regular medications that you take on a regular daily basis? It happens when seizures are different or happen more than usual. The doctor is going to prescribe rescue medications. These medications can be given to non-medical people outside of the hospital and must be given exactly as prescribed. You may use rescue therapy for a child known to you if you have been shown how to use it. It doesn't take the place of the usual seizure medication.
One study revealed that the administration of rescue medication is recommended for caregivers, such as preschool teachers, and should be able to be given correctly to children. In another study, they provided training to 210 preschool teachers from 115 different schools and gauged the level of comfort or confidence in giving rescue types of medication. The results were very positive after their training as their confidence level rose significantly and they committed fewer errors in the practice sessions when they were practicing giving these meds. I really encourage facility directors to seek out this type of training. You can be trained by a skilled parent, a nurse, or a doctor.
Ways to Give Medication
Generally, AEDs that you might take on a regular basis are in pill form, but when there's a seizure going on sometimes more is needed. Medications come in different forms and ways to give them. One way is nasal sprays. Generally, a nasal spray has just one dose of medicine in it and is for breakthrough seizures. Pills can be also given by putting them right inside the cheek, even during a seizure. Also, there are some suppositories that you can place in the rectum.
Additional Treatments
Epilepsy Surgery/Implantation Stimulation Devices
Other treatment options include epilepsy surgery and implantation stimulation devices. Surgery may be done to resect or take out part of the brain where the seizures occur. There's also laser surgery that pinpoints a specific area during surgery. The surgeries are complex and are definitely not for everyone. There is also a vagus nerve stimulation device which is a wire that goes into the brain and passes through to a battery that is put in place in the chest. This battery sends out small energy pulses to the brain to inhibit or stop the seizure activity. When you hold a magnet over that battery it triggers the device to initiate the impulses. These are for children 12 years of age and older who have uncontrolled seizures. This is another intervention to help control seizures. The side effects for having this type of a device for children include a hoarse voice, a sore throat, or just a change in the sound of their voice.
Ketogenic Diet
The ketogenic diet is one of the diets that's used to help prevent seizures. Other diets include the modified Atkins diet and a low glycemic diet. Low glycemic means a low blood sugar diet. The ketogenic diet has been used to treat epilepsy since the 1920s. It's high fat, low carbohydrate, and must be strictly followed. It creates ketones in the body. The brain and heart work normally with ketones for energy.
The brain also uses carbohydrates for energy, but too many carbohydrates are bad for an individual with seizures. The keto diet inhibits those electrical impulses, reducing seizure frequency. Studies have shown that some children become seizure-free when using this diet. Other diets also have shown that there is about a 50% reduction in the seizure frequency with the keto diet and the modified Atkins diet especially. These special diets can be a challenge for families, especially when you have to feed other people in the family. Sticking to a strict diet is difficult so you need support.
Cannabidiol (CBD)
Cannabidiol is the non-psychoactive component of marijuana. The psychoactive component, the part that makes you high, is THC, tetrahydrocannabinol. There are historical records that show the use of cannabidiol in ancient times in 2700 BC before Christ was born. Throughout history, cannabidiol has been used to treat seizures. In the 19th century, there were several physicians that led the charge in publishing papers on its use as an anti-convulsant. There has been a lot of anecdotal and scientific evidence that it is useful in treating seizures in children, as a complementary intervention. In the last decade, social media, family advocacy, and internet activity have led to a significant interest in CBD for epilepsy treatment, especially in children. Many studies surveyed parents who belong to Facebook groups and online surveys and that use CBD to treat their child's seizures. Overall, 80% of parents reported a reduction in seizure frequency. On average, 14% reported a positive effect, and their child became seizure-free.
Mindfulness-Based Therapy
Mindfulness is purposefully bringing one's attention to the present moment and calmly acknowledging and accepting the feelings, thoughts, and bodily sensations you are having at that moment. We use mindfulness-based therapies for women with breast cancer, health care providers under great stress, and people with stomach disorders. There's a lot of research about using mindfulness. One study included children with epilepsy 4-10 years of age and their families. Statistics show that 80% of children with epilepsy have cognitive and mental health disorders, and 50% of parents are at risk of depression. The family environment has a greater influence on the quality of life and mental health than any epilepsy-related issues.
Making Mindfulness Matter (M3)
Making Mindfulness Matter is a program that was developed for parents and children. The question was, can mindfulness benefit individuals? Can it improve the child's and parents' quality of life and their mental health? These interventions must be implemented early. This type of program can be a very low-cost and sustainable program with the help of epilepsy support centers around. In reality, when you go to the doctor for a neurological visit, they take care of the diagnosis, classify what type of epilepsy the child has, and give the medical treatment, but they fail to address the parents' and child's unmet needs.
A parent and child's relationship can suffer, the parent's confidence in their parenting can suffer, and it's very stressful for the entire family. The Making Mindfulness Matter intervention used this outline, which is what they went over with the parents and the children.
- Introduction to brain, breathing, and mindfulness
- How brains work under stress
- Mindful awareness/mindful breathing
- Mindful sensing
- Mindful movement
- Perspective-taking
- Choosing optimism and appreciating happy experiences
- Expressing gratitude and acts of kindness
They talked about the brain, breathing, and mindfulness as well as how the brain, thoughts, and feelings worked together. They talked about how the brain works under stress and what's happening in what part of the brain when that's happening. They also taught about mindfulness awareness and mindful breathing. Slow, deep breathing can take you from a stressful situation into a normal, relaxed state just by breathing. They talked about mindful sensing and did activities with all the different five senses, helping individuals to understand this mindfulness concept.
Thinking about mindful movement, good posture relates to good thinking. They also talked about having a good perspective when things are disruptive and bad things are happening. They did activities related to that and chose optimism and appreciating happy experiences. They did activities that expressed gratitude and acts of kindness. All of this helped these parents and children turn around and have a better experience in their times of trial.
Living with Epilepsy
Challenges
There are many challenges for individuals and families living with epilepsy. This includes all the side effects I mentioned before, other health problems, emotional and social challenges, insurance, finances, and housing. These things can become a burden. There is often stigma for the child, discrimination, and fear. Bullying is a real problem as well. Caregiver stress and isolation occur often because of not wanting to go out when there could be an impending seizure. Work, driving, and play also can be a challenge for individuals.
Thinking about parents' challenges, one study showed that 42% of parents reported high levels of depression, 31% reported high levels of anger, and 77% admitted their social life was disrupted due to their child's epilepsy. They didn't watch TV, go to movies, or spend time with friends. The report also looked at the severe economic burden including 96% from drug costs, 83% from doctors fees, and 22% from hospitalization. These are the burdens that our parents feel.
Strategies for Parents
There are several strategies for parents of children with epilepsy. Common sense, intuition, and experience can help guide in caring for a child with seizures. Research the condition and keep a positive attitude. While it's easy to be overprotective, it's best to avoid that. I was so overprotective of my husband when he had start having some breakthrough seizures. Be open and honest with friends and family.
Tips for All Caregivers
Do not assume that epilepsy is the cause of behavioral problems. It is possible that learning difficulties and behavior may be caused by the severity or type of seizures, brain damage, and certain medications. However, it is important to ask for professional help in finding the cause. Bullying by peers can occur due to a lack of understanding. The child may not be able to assert himself. Some of the signs of bullying include temper tantrums, violence, truancy, not wanting to come to school, and nervousness. Communicate with the child's parent, the caregiver, or the teacher. Support and encourage the child making sure you support them in front of the other children. Do your best to explain to the other children.
Research
Research shows that there's a high likelihood of seizures happening in school. There's often an unexpected decline in school performance. Lapses in concentration might be the first signs of epilepsy in a child you're caring for. The policies at your facility should address the safety and administration of rescue medications for prolonged seizures. Be sure to have a Seizure Action Plan in place for any child who has seizures.
To learn more about epilepsy go to epilepsy.com, call the Epilepsy Foundation, or contact your local Epilepsy Foundation.
Resources
- https://www.epilepsy.com/living-epilepsy/seizure-first-aid-and-safety/first-aid-seizures-stay-safe-side?utm_medium=pdf&utm_source=efa&utm_campaign=toolkit-difficult-treat-seizure
- https://www.stanfordchildrens.org/en/service/epilepsy
- https://learn.epilepsy.com/courses/schools-and-seizure-preparedness-on-demand
- https://www.mayoclinic.org
- Temporal lobe epilepsy
- Reflex epilepsy
- Psychomotor epilepsy
- Intractable epilepsy
- Photosensitive epilepsy
- Traumatic epilepsy
References
Ben-Zeev, B. (2020). Medical cannabis for intractable epilepsy in childhood: A review. Rambam Maimonides medical journal, 11(1), e0004. https://doi.org/10.5041/RMMJ.10387
Detrick, A. (2021). Complementary and alternative medicine (CAM) for individuals with epilepsy. Honors Undergraduate Theses. 992.
Dumeier, H. K., Neininger, M. P., Kaune, A., Schumacher, P. M., Merkenschlager, A., Kiess, W., ... & Bertsche, A. (2017). Seizure management by preschool teachers: a training concept focussing on practical skills. Seizure, 50, 38-42.
Elliott, J., DeJean, D., Clifford, T., Coyle, D., Potter, B., Skidmore, B., ... & Wells, G. A. (2018). Cannabis for pediatric epilepsy: protocol for a living systematic review. Systematic reviews, 7(1), 1-5.
Hussain, M. M., Zulfiqar, Z., Ishfaq, K., & Ghaffari, A. S. (2021). Psycho-social and economic problems faced by parents of children with epilepsy. Review of Education, Administration & LAW, 4(2), 521-530.
Iannone, L. F., Roberti, R., Arena, G., Mammone, S., Pulitano, P., De Sarro, G., ... & Russo, E. (2021). Assessing knowledge and attitudes toward epilepsy among schoolteachers and students: Implications for inclusion and safety in the educational system. PloS one, 16(4), e0249681.
Laino, D., Mencaroni, E., & Esposito, S. (2018). Management of pediatric febrile seizures. International journal of environmental research and public health, 15(10), 2232.
Sourbron, J., Klinkenberg, S., van Kuijk, S. M., Lagae, L., Lambrechts, D., Braakman, H. M., & Majoie, M. (2020). Ketogenic diet for the treatment of pediatric epilepsy: review and meta-analysis. Child's Nervous System, 36(6), 1099-1109.
Tang, V., Poon, W. S., & Kwan, P. (2015). Mindfulness-based therapy for drug-resistant epilepsy: an assessor-blinded randomized trial. Neurology, 85(13), 1100-1107.
Citation
Nathenson, N. (2022). Seizures and seizure management in early childhood. Continued.com - Early Childhood Education, Article 23797. Available at www.continued.com/early-childhood-education
