Editor’s note: This text-based course is an edited transcript of the webinar, Caring for the High Anxiety Pulmonary Patient and Family, presented by Nancy A. Nathenson, RRT.
Learning Outcomes
After this course, participants will be able to:
- Explain the four key components of anxiety.
- Describe the factors that affect anxiety levels in the pulmonary patient that can and cannot be changed.
- Identify examples of biomedical and holistic interventions to reduce anxiety in the pulmonary patient.
- Define the role of “therapeutic use of self” in managing anxiety in the pulmonary patient.
What is Anxiety?
Anxiety is a response to danger. For an anxious pulmonary patient, even normal activity can pose a threat to them. Anxiety is a feeling of dread, fear, and/or lack of control as a normal or protective response to a perceived threat to our homeostasis. It is an unpleasant complex combination of emotions and physical sensations, such as heart palpitations, nausea, angina, and shortness of breath. All of these things can manifest in an anxious patient.
Other manifestations that our patients can experience due to anxiety include worry, frustration, tension, panic, and fatigue. They may be scared or negative in their mood. They could be depressed and overwhelmed. They could be nervous or suffer from insomnia. All of these things are potential symptoms of anxiety in our patients.
Components
What are the components of anxiety? Anxiety can be physiological, emotional, cognitive, or behavioral. It is often difficult to determine if it is anxiety, high CO2, or other medical factors that might be the cause, such as medication interactions. There are multiple perspectives when we think about our patient that is anxious. We have the staff's perspective of what is going on, the family member's perspective, and also the patient’s perspective. It is a delicate balance to manage the anxiousness of a patient with all of these perspectives being involved.
Not all anxiety is created equal. Anxiety can be acute, chronic, or generalized. Acute is something immediate, while chronic anxiety is continuous. It could also be a symptom of pulmonary disorders as well as a cause of pulmonary hypertension symptoms. The more anxious you get the more pulmonary hypertension symptoms could occur. Generalized anxiety lasts more than six months without any other comorbidity being involved. It is not a pulmonary issue or condition that is manifesting.
Pulmonary Patients
You may be wondering if pulmonary anxiety is different. The answer is yes and no. The danger for our patients is or has been, real. The body is not able to function normally and the behaviors may be even more resistant to change. However, it is not so different than other anxieties because the physiological signals are essentially identical. The thoughts and emotions that patients experience are essentially identical.
Depression is one of the most common mental illnesses in the elderly. It includes emotional, cognitive, and behavioral symptoms. Our patients often feel breathless and avoid activities that make them feel breathless. When they do less, their muscles weaken. Then they get more breathless, feel depressed, and avoid activities that make them feel breathless. It is a vicious cycle for our pulmonary patients that are struggling to breathe and to do the activities that they enjoy.
Studies show that anxiety and depression are more common in COPD patients compared to the general population. COPD patients are 85% more likely to develop anxiety disorders than healthy persons. This anxiety is associated with dyspnea, with their inability to perform their activities of daily living or fulfill their social role as a parent or a grandparent. It is also associated with rehospitalizations.
A recent study showed that individuals with asthma (25-49%) are significantly more likely to have symptoms of anxiety and depression. Anxiety and depression symptoms have differential effects on dyspnea over our patients. There are implications for our understanding of how psychological states influence asthma control. Also, physicians need to consider the psychological state of the patient before establishing a treatment regimen for them.
Asthma is the leading chronic illness for children and adolescents. Research shows that between psychological disorders and pediatric asthma there is evidence of disorders of anxiety three times higher than in children without asthma.
COPD patients have a high rate of panic anxiety. Repeated dyspnea and exacerbations cause this type of anxiety, as do hypercapnia and hyperventilation. The stress of just having a chronic disease can cause panic anxiety. Anxiogenic medications are medications that cause anxiety. Although benzodiazepines are used to treat anxiety, if there is an abuse of that medication it can cause the reverse effect and be anxiogenic in nature. There are substances that cause anxiety such as cocaine, certain foods, and caffeine. These are anxiogenic substances.
Panic anxiety carries significant morbidity. Avoidance of activity, over-medicating with benzodiazepines, and prolonged hospitalization are factors. Remember that panic attacks are sudden, not gradual.
In pulmonary hypertension patients, perceived dyspnea is associated with anxiety, but not depression. Anxiety is underdiagnosed and undertreated in pulmonary hypertension patients, especially those without a history of anxiety or depression. That psychological factor is not considered when a patient has a new diagnosis of pulmonary hypertension.
Pulmonary hypertension affects the lungs and the right side of the heart. Pulmonary arterial hypertension, on the other hand, is when the blood vessels are narrow, blocked, or even destroyed. In a study by Chan, patients most frequently associated their anxiety with the inability to communicate, difficulty sleeping, and distorted perceptions. Think about the mechanical ventilator patient that is unable to use the speaking valve and unable to communicate verbally. The incidents rates of anxiety in those patients range from 30 to 80%. This number may be significantly higher because the reports are predominantly from patients that have survived the ICU, are cognitively intact, and are able to communicate about and reflect on their experience.
Impact of Anxiety on Recovery
Prolonged Mechanical Ventilation
Prolonged mechanical ventilation is the biggest consequence of anxiety. High levels of anxiety result in more ventilator days, 14 versus 6. We are definitely not going to be able to be weaning our patients as we like. High levels of anxiety result in longer lengths of stay, from 12 in this study versus five. Prolonged mechanical ventilation may also result in ventilator-acquired pneumonia, malnutrition, PTSD, or depression.
Device Disruption
Anxious or agitated patients are more likely to self-extubate, decannulate, pull off their high flow nasal oxygen, or pull out their catheter or NG tubes. This increases the risk of infection, injury, or other medical complications. When respiratory rates are above therapeutic levels, patients are unable to participate in therapy. They are unable to trial the speaking valve and unable to wean from the mechanical ventilator or the tracheostomy tube.
Anxiety and the Immune System
In addition, anxiety affects the immune system. Anxiety is stress, which affects the immune system, as well as all of our other systems. Even just a few minutes of anxiety or stress can inhibit the first responder activity of the immune system. The first responders of the immune system are the macrophages, the T-cells, and the B-cells that destroy pathogens. They just gobble them up. There are anti-microbial peptides that are released before the macrophages and the T and the B-cells are able to respond as a first responder for this type of stress and anxiety. Chronic anxiety weakens all types of immune responses. Elderly people, of those already ill, are more prone to stress and stress-related immune changes.
Anxiety and the Heart
Anxiety also has an effect on the heart. Eighty percent of those experiencing panic list rapid or irregular heart rate as a symptom. This may increase the risk of cardiac arrest. Chronic anxiety is related to a 26% increase in coronary heart disease. Anxiety also results in increased blood pressure, which weakens the heart muscle and increases the risk of coronary heart disease and stroke.
Recognizing Anxiety
Sometimes it is very easy to recognize anxiety in our patients. However, anxiety symptoms are typically reported verbally. Medically complex patients, including patients on ventilators or those that are sedated, often are unable to do that. They are unable to voice their symptoms. The accuracy of interpreting observable clues is confounded by pain, delirium, medical status, and their inability to communicate. Some of my patients have said things like, I cannot think straight, I do not remember, my heart is racing, I am sweating, I cannot relax, I cannot sleep, or I am scared.
Physiological or Somatic Signs
The physiological or somatic signs are our vital signs. This includes tachycardia, hypertension, tachypnea, sweating, and abdominal stress. These can all be signs of anxiety in patients.
Behavioral Signs
Some behavioral signs of anxiety include large muscle group movement, such as when patients are kicking, attempting to stand or sit up, or striking out or thrashing. Other behavioral signs include small muscle group movements such as picking at the sheets or bandages and rhythmic head movements such as tossing their head back and forth. In addition, grimacing, trembling, crying, or increased complaints by the patient can be signs of anxiety.
Psychological Signs
Some of the psychological signs of anxiety include sadness, being withdrawn, or being angry. Patients can be hypervigilant, watching every move we make. They may distrust us and be very fearful. They also might have an unrealistic perception of their situation or express feelings of loss of control.
Factors that Affect Level of Anxiety
There are factors that can affect the level of anxiety in our patients, but they cannot be changed. This includes the patient's medical history, such as their history of respiratory failure, and their medical experience prior to admission. We cannot change what experience they may have had. There is a high base rate of anxiety (30%) in the general. There is a genetic predisposition for an anxious or timid temperament. A person’s temperament cannot be changed. Their early learning history, including what they have learned about their condition, cannot be changed, nor can any kind of substance abuse history.
What are the changeable factors of anxiety in our patient? We can work on changing their thoughts or beliefs. We can change their respiratory status with breathing treatments, coaching, ventilator weaning, and oxygen. We can also change their arousal levels, such as their excitability or nervousness. We have multiple ways of doing that.
Interventions
Our overall goal for the patient is to assist them and their family in relearning a sense of safety in the frightening situation that they are in. This situation may be still life-threatening for the patient. We want to lower the stress and arousal for the patient and family. To do this they must trust you and they must trust the team. There are many things that we can do when we are providing breathing treatments, ventilator weaning, and other services.
There are many interventions we can do. These include cognitive and emotional, which is going to involve the brain, behavioral, and social and environmental, which might involve friends and family. There are physiological interventions, which is where biomedical and holistic options come in play. There is also the therapeutic use of yourself for patients.
Cognitive
One cognitive intervention is cognitive behavioral therapy (CBT). CBT is a therapy that is well-researched and is very effective for PTSD, anxiety, and many other psychological conditions. It is an evidence-based, nonpharmacologic treatment that explores the relationship between a person's thoughts, feelings, and behaviors or actions. Cognitive behavioral therapy helps an individual put a stop to the thoughts that lead them to anxiety and replace those thoughts with realistic and rational thoughts so that when these self-statements are practiced and learned, the brain takes over automatically. This is a form of conditioning, meaning that brain chemistry (neurotransmission) actually changes as a result of new thinking habits. Patients definitely have to be alert and cognitively able to participate in this so that they may practice these statements.
To help retrain the brain, here are some statements that patients can say to themselves when they are particularly anxious. These will help patients reassure themselves that they are going to be okay. They must practice these statements so they become second nature.
- I already pressed the call light and they will come – pressing it again will only exacerbate my anxiety. I will try instead to distract or focus on my breathing.
- I am having a difficult time breathing and that is why my body is physically reacting like this. Thinking the worst is only going to add to these physical reactions and make it even harder to breathe.
- I am going to be alright. I am just going to relax, calm down, and everything will be alright.
- Right now, I have some feelings I don’t like, and that is ok. Anxiety will pass and it will not last forever.
There are other cognitive interventions we can use to identify and modify the catastrophic thoughts of our patients. We can do this through education. Always educate the patient at every interaction and be consistent in your messaging to them. Have confidence. Work as a team to help patients. Be sure to talk to patients while you work and explain what you are doing. Ask permission to touch the patient and to do different things as you work with them. Provide information on the reasons for the physical sensations that they might have and take time to explain the alarm sounds and the nurse call sounds.
Emotional
Emotional interventions include having a nurturing attitude and a low-key, non-defensive style. Respond to and do not ignore patient questions. During personal interactions with patients be trustworthy and reliable. If you say you are coming back to give them their breathing treatment at eight o'clock, come back at eight o'clock. Show them that you can be reliable. Again, remember to ask permission and explain things. Be cheerful and distracting. Use your personality and be your best self when you are with your patients. Make sure to validate their experience and to never patronize them.
Behavioral
We want to stay calm and detached from patients and not get too personally involved. If the patient has a complaint, is it valid? Be proactive and solution-focused. It is very important to identify one family point of contact and give the family one primary staff to contact per shift. This is usually a team decision. When patients behave appropriately, reward the desired behavior with kudos and praise. Limit your responses to undesirable behavior, such as a patient that is constantly pushing their call light.
Decrease their sense of helplessness by orienting them to their level of care, whether they are in ICU or in a subacute unit. Let them know that we know how to tell if the patient is in a real crisis and we can manage that. Teach patients ways to decrease their anxiety, such as coaching their breathing or distracting them. If the patient is able to leave, they could go for a car ride. I came from a rehab hospital where this happened all the time. Provide them with information on their respiratory status, weaning, and treatments that are consistent, simple, and repeated as many times as necessary. The care plan is going to be key to describing what you are going to be doing with the patient and being consistent. The more information they have, the less anxious they will be.
Social/Environmental
Social/environmental modifications such as removing or modifying stimuli, whether positive or negative, can reduce anxiety. This may be having the TV volume too loud while watching a football game or a family that is talking loud or having discussions that could be perceived as being upsetting. Place the monitors in or out of the patient's line of sight, whichever will help them stay calm. That is different for every one of our patients. Some patients are very obsessed with looking at the oximeter and some not so. We want to distract them and disengage their negative thoughts by chatting with them or having them watch TV or listen to music. Place pictures or decorations from home in their environment that can uplift the patient. Sometimes patients are often not able to evaluate risks due to cognitive and perceptual dysfunction, which is just part of their illness. Normal activities may be perceived as threats.
Befriending is a telephone-based contact program that focuses on everyday conversation topics delivered by trained and supervised volunteers. This is to follow up with our pulmonary patients to see how we might be able to make sure that they are taking good care of themselves at home, they do not come back to the hospital, and they are able to do their activities of daily living and the things they enjoy.
Research showed that befriending can assist in reducing anxiety and depression in COPD. Touching base with a phone call is not a substitute for professional psychological services, but it can be useful for patients who are waiting for professional services or after their treatment course.
Oftentimes when patients are released from the emergency room or the hospital they cannot get in to see the psychologist for a while. Syeda, Trucks, and Sears (2018) did a study at the VA in Boston Healthcare System targeting veteran patients that had been hospitalized for COPD. They used telephonic outreach in the pulmonary service (TOPS) for those patients who had been hospitalized as a type of befriending. The results of this befriending study showed improved access to ambulatory care and a reduction in the rate of readmissions after a nurse-directed telephone outreach intervention.
In a study of COPD patients with mild to severe anxiety, a group received telephone-based befriending and cognitive behavioral therapy at the same time. They had better outcomes with anxiety and depression, as compared to a control group that received the usual care and just the befriending phone call. Of all of the cases, 42% had less anxiety and depression. Researchers recommended telephone-based and cognitive behavioral therapy as a preventative measure and as being cost-effective.
Physiological
There are several physiological interventions that respiratory therapists do. This is where we shine. Every day, day in and day out, we work on improving the respiratory status of our patients through managing their oxygenation, making sure that they do not have too much or too little. We manage their ventilation by assessing their work of breathing every time we interact with them. We constantly monitor that.
If there are work of breathing issues, we will adjust the ventilator settings. Perhaps the mode needs to change. We can adjust those comfort settings to help the patients get their breath more easily. We may consider repositioning them and make sure when we leave them or when we are giving their treatment they are in a really good breathing position that is going to help them ventilate well.
In addition, we will tailor each ventilator or weaning strategy specifically to the patient’s needs. It is going to be individualized. Research has shown that when you incorporate ventilator or tracheostomy weaning protocols that these types of interventions can decrease mortality, decrease the length of stay, decrease the patient’s cost, and provide savings for the hospital. Some studies show that it can decrease ventilator-associated pneumonia incidents.
The types of ventilator weaning protocols that have been studied are when you use non-invasive ventilation, from the ventilator to liberation, or heated high flow as a bridge from ventilator dependence to liberation. For almost everyone, the strongest response is going to be to medications and treatments. This will decrease their air hunger. They are going to feel better because they are going to be able to decrease their agitation and anxiety because they are catching their breath better.
My Holistic Background
Now I will share with you a little bit of my holistic background because we are going to be talking about different physiological interventions that are holistic in nature. I have a personal story to share in regards to that. Hopefully, by sharing this with you, it will give me some street creds so you will feel like I know what I am talking about.
I became a certified holistic life coach in 2010. In 2012, I was certified level two in lymphatic enhancement technology, which is a technology that helps to mobilize the lymphatic system. In 2013, I became a registered yoga teacher. I have taught restorative yoga to stroke patients at my rehab facility. I also taught yoga, meditation, and aromatherapy to the English as a second language parents at the local public school.
The other thing that interested me was meditation. I was a meditation teacher and facilitator with my partner and husband from 2012 through 2020. I am also the owner and practitioner of a wellness practice with my partner since 2010. We do that together. He is a nurse practitioner and a natural medicine doctor, or a naturopath. I also have a passion for women's wellness and self-care, which I have shared with a variety of support groups, such as breast cancer and brain cancer support.
My personal backstory has to do with how my husband and I both came to be interested in natural medicine and holistic practices. My husband, who was an administrator at our facility, had a primary brain tumor called an oligodendroglioma. I am happy to say he is a cancer survivor. He had surgery and they were able to resect it but it was not a complete and total resection. We were concerned about recurrence, and sure enough, the cancer came back. When he had his first diagnosis, we did some of these types of holistic interventions that I am going to talk about, including aromatherapy, meditation, music, massage, and things of that nature. He also did what is called the cancer diet. Diet is a big part, but these holistic interventions were a big part of our lives as well and helped us handle the anxiety and stress that we were under.
I speak from a caregiver perspective, and as one that experienced with my husband that anxiety and fear during his recovery. I remember him being so anxious when he knew he was going to have to try to do steps one day. He became hemiplegic and was very fearful about doing steps. He used to cry about speech therapy because he could never remember the name of pineapple. He had a hard time making change and doing word problems. That was always very overwhelming for him.
My anxiety and my stress manifested in other ways. For example, on my way home one night I drove home twice and I got to an intersection and I did not know where I was on the planet. I would see him at work because I worked at the same facility, and I would see him struggling with his rehab. That was a big stressor. Within his recovery time, we worked really hard at decreasing our stress and anxiety. We did that together. We started some of these interventions while he was in the hospital.
I am happy to say he is cancer-free. He said he was not going to have surgery and he decided to do a natural approach. That is when he started all the different holistic interventions and diets and he has been cancer-free for many years.
What is Holistic Health?
Holistic health is a wellness approach that cares for the whole person, including the body, mind, spirit, and social needs. It is based on the understanding that all of these aspects affect your overall health. When you are unwell in one particular aspect, it affects you in others. When our body is suffering, it can affect our mind. When our mind is suffering it can affect our social situation and our social relationships. How can we care for our patients and families with this approach in mind or at least guide them? I am going to give you some tips on what we can do as clinicians at the bedside, for our patients and families, but also for ourselves.
Stress is the thing that we battle the most in healthcare and with these particular patients. Think about the stress cycle. Cortisol is the steroid hormone that is secreted by the adrenal cortex in response to stress. Cortisol increases blood pressure, increases blood sugar, and suppresses the immune system. There is sympathetic fight or flight in the nervous system and parasympathetic, which is the relaxation response. You can only be in one at a time. You are either in a sympathetic fight or flight or parasympathetic relaxation response.
Think about a day like this. You are on your way to work and you are running late. You find out that you have your performance evaluation that day. Someone called in sick. You never have time to recover from the stressful situations that are just building upon themselves and the anxiety that comes with those events. This is what we are going to work on.
Holistic Interventions
The holistic interventions we are going to discuss today are easily accessible and are low or no-cost interventions. We will begin with aromatherapy, then talk about music, meditation, guided imagery, and Comfort Touch, which is an easily teachable massage intervention. With holistic interventions, as with the rest of healthcare and how we deliver care, it is important to use our intention and our intuition.
Intention is used by the caregiver to set the environment for healing and wellbeing. We do that in how we treat the patient and how we care for them. We should listen to our intuition and not ignore our inner wisdom. We should not ignore those gut feelings and the intuitiveness we have when we care for our patients and their well-being. It is something that is very powerful.
Aromatherapy
We are going to start with aromatherapy and some fun facts about it. Aromatherapy is a simple intervention that has been around for thousands of years. It began being used as early as 7,000 BC in Egypt where olive and sesame oils were added to fats and were used as poultices. In the Middle East around 2800 BC, kings and queens would have expeditions to the African coast to obtain frankincense and myrrh trees.
In Greece around 700 BC, Socrates worried that perfumes would blur the lines between slaves and free men, as slaves smelled of sweat, and free men did not. When Christ was born, frankincense and myrrh, which the three kings brought to baby Jesus, was more expensive than gold. During the Roman ages around 800 AD, they used 2,800 pounds of frankincense and 250 pounds of myrrh per year. There is documentation of these elaborate activities, parties, and celebrations where hundreds of thousands of dollars were used for aromatherapy.
People in the Orient around 1100 AD believed that plant extractions liberated the soul. In Japan, they used cinnamon incense in the sleeves of kimonos and robes to enhance the odor of the kimono. In Muslim culture, rose was the preferred scent. Their temples were filled with a rose scent and they made prayer beads out of rose. The nuns and monks at that time guarded what they called the miracle water, which was the aromatherapy oils that they used in water.
By the time Christopher Columbus hit American soil around 1400, cedarwood and vanilla were a couple of the scents that were used quite often. Native Americans had a long history of using aromatherapy. The Incas used an ointment that had valerian root, which is a supplement that is used for muscle spasms. It is one that my husband uses when he has muscle spasms because he is hemiplegic.
In the 1800s, the Paris International Festival introduced soaps and perfumes separate from the pharmacy. France was the leader in the therapeutic use of aromatherapy. A gentleman named Gattefosse coined the term aromatherapy in France. In 1977, a gentleman called Tisserand wrote The Art of Aromatherapy which is what launched aromatherapy, into a very disciplined healing art.
One part of aromatherapy is essential oils, which are the essence of a flower or a plant. They can affect our mood and how we think or feel at any given time. They can provide a variety of health benefits, such as physical, mental, emotional, and spiritual balance. Aromatherapy can be put on topically, inhaled, and in many cases, you can drink the oils with water.
There are different scents that have different healing properties and have proven effects on the brain and body. Scents can evoke long-term memories, which can be good or bad. Sensitivity to a scent is largely cultural. For example, I do not like the smell of curry, but I definitely like the smell of corn on the cob. Maybe fried okra does not resonate with you, but other scents do. If you do not like a smell it is not going to be therapeutic for you. Even if lavender has been shown to be very effective for different conditions if you do not like the smell it is not going to work for you.
Aromatherapy can be a very powerful intervention for stress reduction. That is because of the interrelationship it has with the limbic system. The limbic system in your brain controls emotions and influences the nervous system and hormones. It is the center of emotions, memory, and arousal.
The oils are transmitted through the olfactory nerve, which goes straight to your limbic system. It does not have to go through the spinal cord for processing at all. They affect heart rate, stress level, blood pressure, breathing, memory, digestion, and the immune system. Your brain cannot help but respond to aromatherapy and to the scent. When the hypothalamus receives the input to relax, neurochemicals are released and sent through the body to relax and calm.
Lavender. Lavender is not my favorite scent, but it has been found to have calming, relaxing, stress-relieving, and healing properties. I use lavender oil on cuts and burns and it works very well. In fact, most essential oils have an antibiotic component to them. Lavender can be effective against insomnia, headaches, and anxiety.
A study in an acute care setting across a large hospital system measured patient-reported anxiety, pain, and nausea before and after receiving aromatherapy. The results revealed that after the nurse delivered aromatherapy through essential oils the pain, anxiety, and nausea were reduced. Additionally, there was a significant reduction in anxiety that occurred in one particular ICU setting. Keep in mind, this was across a huge hospital system. Lavender was the most frequently used in this study and it was used via inhalation or diffusing. Diffusing is one way to deliver aromatherapy.
Bergamot. Bergamot is one of my favorite scents. It is a light citrus aroma that helps to uplift the spirit and assists with anxiety and compulsive behavior. Bergamot can help the patients we talked about earlier who would pick at their sheets, tubing, or dressing.
One study showed that for pre-surgical patients, regardless of the patient's surgical experience, the patients that were exposed to bergamot were less anxious and had lower heart rate and blood pressure than the control group that did not experience that. These were measured while they were waiting for their surgery.
Frankincense. Frankincense is my favorite scent. It is a woodsy smell that is very subtle. Frankincense is what my husband and I used. We used it when we meditated and at night for sleep. We used it in the hospital when he was an inpatient. It helps to calm and center the mind. Frankincense also helps to ease that mental chatter, agitation, and worry.
The Dalai Lama says that the mind is an unruly child. When you are anxious, your mind is not perseverating on positive things that are happening, but it focuses on negative things. When you have increased anxiety, you have the negative effect of unproductive worrying which represents an unsuccessful attempt to control the perceived danger. Frankincense is very good for that. It is a little bit on the expensive side, but very therapeutic and powerful.
Peppermint. Peppermint helps to counteract shock, mental fogginess, and lack of focus. It helps to calm nerves. Peppermint also helps with coughs and colds. It is a very uplifting smell. It has also been studied quite a lot. One study showed that peppermint aromatherapy can decrease the level of anxiety before undergoing a colonoscopy. It is recommended to employ this non-pharmacologic, low-risk, pleasant method of aromatherapy for patients before invasive procedures such as colonoscopies.
There are many applications for the use of aromatherapy and how effective it can be.
Holistic Interventions Program
I had a very unique opportunity and role at my rehab facility to develop programs. One of those programs was the holistic interventions program. This arose out of my husband's time at the hospital. Keep in mind he was an administrator at our rehab facility and he was there actually for six weeks of rehab and then came back for outpatient for many months after that.
I was charged with starting a holistic interventions program. The purpose was to include aromatherapy and music for any patient as a non-pharmacologic approach to pain and anxiety. When I started this program, I needed administrative buy-in. Thankfully we had that because we had administrators that were in support of my husband and some of the things that he was doing for his anxiety, pain, and stress. We identified champions on the units to help support the program.
We developed a policy that was very clear that we would reach for aromatherapy and music as an intervention prior to giving a patient a pain med or an anxiety med. Anyone could suggest this, but it was generally deployed by nurses or therapists. We had a procedure lined up and had the kits that had everything in them. We had a process for checking them out and restocking them. We also had documentation that we used.
Figure 1 shows an example of the holistic intervention flow sheet, which is very easy to navigate. We could use aromatherapy, music, or a combination of the two.
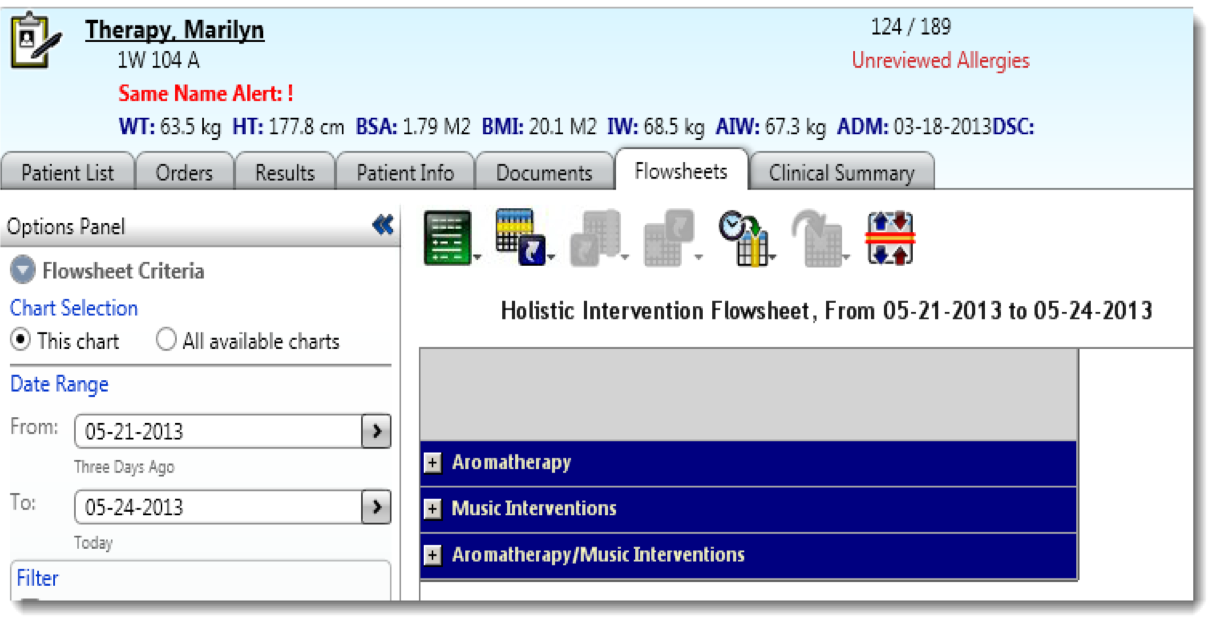
Figure 1. Example of a holistic intervention flowsheet.
Another part of our flow sheet was the indications, as seen in Figure 2.
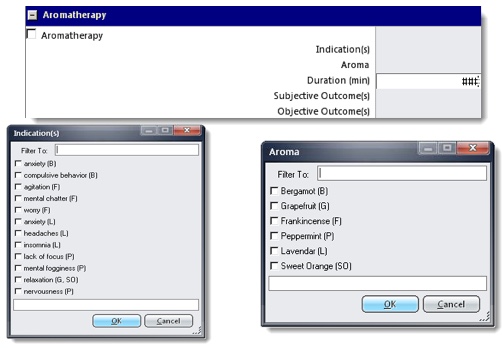
Figure 2. Example of aromatherapy indications.
The indications showed the reason why we were going to be giving this aromatherapy, such as anxiety, and we had the initial of the essential oil next to it. That could also prompt the nurse that was going in there to select the proper essential oil to treat that particular condition. For example, anxiety and compulsive behavior were treated with bergamot while agitation and mental chatter were treated with frankincense. Headaches and insomnia were treated with lavender. We also had a selection box for choosing that type of oil.
Figure 3 shows the subjective and objective outcomes we were looking for from using aromatherapy.
Figure 3. Example of aromatherapy outcomes.
For example, subjective outcomes would be to have the patient be more relaxed, more focused, or to have a positive behavior change. If a patient was constantly on their call light and we wanted to try to curb that behavior, we might try aromatherapy. Objective outcomes included decreasing blood pressure, heart rate, pain, and respiratory rate.
In 2012 we did a study on our long-term care unit with our nursing home residents our special needs units and our subacute unit. We used the holistic cart and gathered data both before and after residents received aromatherapy and music interventions. This was not a formal study. Figure 4 is a graph of some of our outcomes from these interventions.
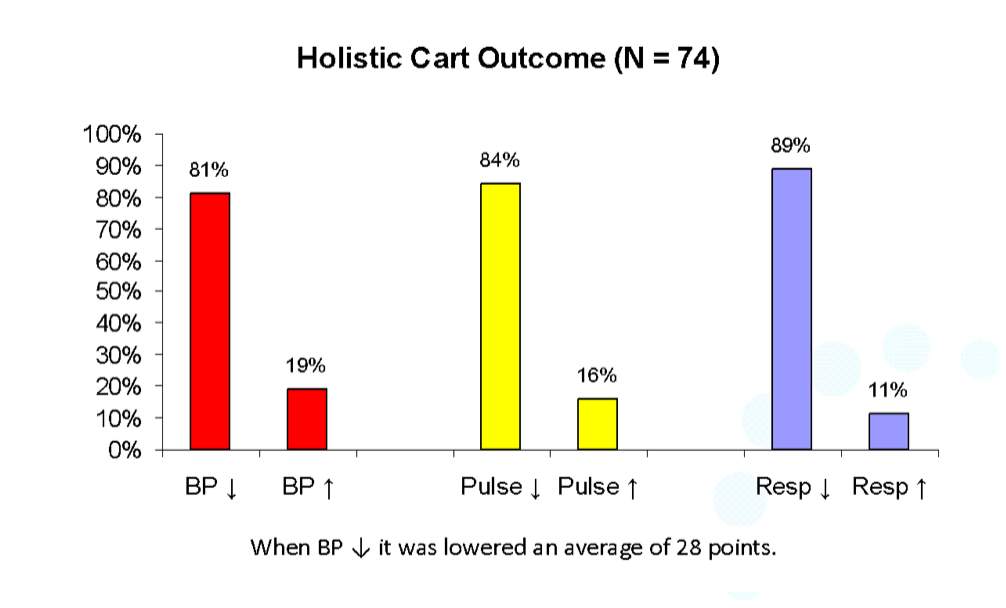
Figure 4. Graph of outcomes from holistic care.
We were looking to see if aromatherapy and music played a part in lowering blood pressure, pulse, and respiration in our patients. Anecdotally, it helped patients immensely. The information we gathered showed that blood pressure, pulse, and respiratory rate were affected in a positive way.
Physiological Interventions
Music is a physiological intervention. Many people are lifted up when they listen to music that they love. Music can also make you sad if you listen to sad music and you are feeling sad. Music acts on your brain like aromatherapy. It heads to the same area of the brain and affects you and your mood.
A study showed that music distracts patient’s attention and decreases their heart rate, blood pressure, respiratory rate, and body temperature. In this study, patients listened to their favorite music for 30 minutes. The study showed a significant decrease in anxiety as measured by the Faces Anxiety Scale.
Music and Relaxation
When stress and anxiety exceed the normal level, the individual loses his or her adaptive power in the situation that they are in, whether it is a perceived threat or a real threat. Music and relaxation can reduce blood pressure and pulse in the elderly. Preferred music listening as a complementary intervention was found to decrease the debilitating effects of anxiety and depression. Music expedited a positive emotional response, provided improved mood, and offered a distraction from current problems. Music is a very powerful tool. I am a very big fan of the big band era but I also love Jethro Tull, Queen, and Lady Gaga. Those types of music really lift me up. Think about the preferred music that a patient might have and consider suggesting that they listen to that type of music.
Another type of music for relaxation is entrainment music. This type of music has been very well-researched by Dr. Jeffrey Thompson, the founder, and director of the Center for Neuroacoustic Research in California. His research is actualizing its vision of healing the body, heart, mind, and spirit through the scientific application of sound. He is considered one of the world's premier sound healing researchers. He uses brain entrainment as a tool for helping individuals come to a more relaxed state to heal the mind, body, and spirit. He is a physician, musician, composer, inventor, educator, and author.
The type of music that he is using relates to all the brainwaves, which are going on at the same time. However, we have one predominant brainwave. The beta waves in our brain are busy waves. These occur when we are actively thinking and problem-solving. We probably all have more beta waves right now as I am presenting to you and you are listening to me and thinking and wondering about this information. When you have more alpha waves in your brain, you are more relaxed, calm, and using creativity. Musicians and artists are sometimes more chill and more relaxed. They have more alpha waves going on in their brain.
When you have more theta waves, that is when you are on the verge of sleep or deep relaxation. The theta wave has been known to be the healing wave and we will talk more about the theta music. At our facility, we had music kits and provided preferred music from jazz to country-western to rock to big band era. We also provided theta music. After a time, we decided to strictly use the theta music for our patients because of its profound impact on the brain, reduction of the increase of the theta waves, and relaxation effect.
You have more delta waves when you are asleep. When you listen to entrainment music, whether it is delta music, theta music, or alpha music, your brainwaves synchronize with the embedded wave in the music. Classical music is naturally theta-based so it is very healing.
Dr. Jeffrey Thompson's music can be found on iTunes or on CDs. The best way to listen to music is with headphones because they will block out all the extra ambient noise around you. The music is beautiful but it is also therapeutic and your brain cannot help but respond to it.
Theta entrainment music helps provide healing of the body. Theta waves communicate to your brain to produce positive chemicals in the brain such as epinephrine and to decrease cortisol, our stress hormone. It can boost the immune system and promote healing. It also balances serotonin, which is your feel-good hormone, and melatonin, which is your sleep hormone. That helps with depression as well as insomnia. Theta music is very powerful music.
Figure 5 shows some screenshots of the documentation that we use for our facility when we were doing music interventions. We identified whether it was a personal choice or theta music, the duration of the music intervention, and the indications.
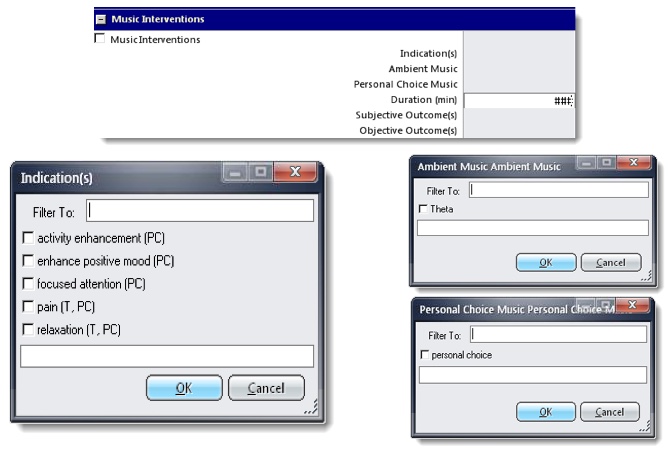
Figure 5. Examples of music interventions.
We also tracked the subjective and objective outcomes, just as we did for the aromatherapy intervention. Figure 6 shows the subjective outcomes such as decreased anxiety, being more focused, increased energy, and being more relaxed. Objective outcomes included decreased blood pressure, heart rate, respiratory rate, and pain.
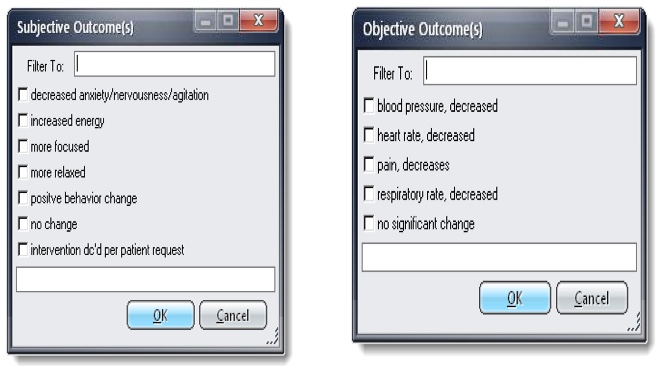
Figure 6. Examples of music interventions outcomes.
Meditation
Meditation comes in many different forms. Just a few minutes of meditation a day can help you do many things. It can help you clear away the information overload that builds up every day and contributes to our stress. It can help us gain a new perspective on stressful situations. Meditation helps you build skills to manage your stress and to increase your self-awareness. It helps you to focus on the present and can also reduce negative emotions.
The benefits of meditation are the same as with many of the interventions I have talked about. Meditation stimulates the parasympathetic or the relaxation response. It decreases heart rate, breathing rate, and blood pressure. It enhances the immune system and promotes healing. Meditation also increases energy and reduces inflammation. This is not a complete list of the physiological impact that meditation has on the body. Inflammation, according to Johns Hopkins, is the basis or the cause of all diseases, from diabetes to asthma to COPD. Inflammation is the cause and meditation decreases inflammation. If it is going to decrease inflammation, it is also in turn going to decrease pain, which is another good effect of meditation.
There are different types of meditation, including mantras, mindfulness, focused, and transcendental meditation. Maharishi Mahesh Yogi is known for developing the transcendental meditation technique, which involves meditating for 20 minutes, twice a day. There are multiple studies that show how it has improved students' scores and their attention.
The most simple types of meditation are the ones we will talk about more. Mantra meditation is when you have a quiet mind and repeat a phrase to yourself. For me, I repeated, “Hail Mary, Full of Grace.” Another mantra is, “I am, all is, one.” That phrase is indicative of the connection that we all have together. There are many different mantras to choose from. When you repeat a mantra in your mind to yourself during meditation time it helps you to concentrate just on that. It also helps you not to have your mind wander off and make grocery lists or things of that nature.
Mindfulness has been in the news and is very mainstream now. It is in elementary and high schools, as well as in healthcare. Mindfulness is when you listen to everything around you and the time between sounds. Listening to what is around you helps you to focus. Focused meditation is when you use an object or a sound or music. We have already talked about how entrainment music can bring you to a meditative state.
A study by the Lung Health Institute in 2016 showed positive effects of meditation on COPD. They had COPD patients that practiced 11 hours of meditation per month. That is less than 30 minutes a day. It improved their mood and lowered their overall anxiety, depression, anger, and fatigue. Quieting the mind for a short time every day has positive impacts. When you are consistent with it you will see the most benefits.
Guided Imagery
Guided imagery is something my husband did and still does, along with meditation. We do our meditations in the morning, and at night I like to use music. When my husband had brain surgery and his recovery and then when his cancer came back, he used guided imagery. That is when you concentrate on a specific object, sound, or experience in order to calm your mind. For him, he imagined was when he lived in Point Arena, California, and he was on the beach near a cave with waves crashing into it. He imagined the cave and the waves lapping back and forth clearing cancer from his brain. He used that to help calm his mind and clear away cancer.
The benefits of guided imagery are the same as we have been talking about for so many of these holistic interventions. It helps with relaxation, reduces stress, and gives you a sense of wellbeing. It can manage negative emotions and improve your coping skills.
You might imagine your safe place as being in a cabin cozy in front of a fire and it is snowing outside, or you are laying on a beach and hear the waves lapping on the shore, or you are floating in a boat looking at the stars at night. Just imagining those situations and experiences can bring you to a state of decreased stress and relaxation.
Resources
There are a lot of free resources for accessing guided imagery and meditation including Insight Timer, Calm, and Headspace. These are places you can find short narratives on experiences and imagery to guide you to a relaxed state.
For music, I really enjoy Pandora, specifically liquid mind. It is beautiful music, never irritating, and easy to pull up on your phone. You can get free versions of Pandora and Spotify. I believe they may have ads in them but they are free and accessible. You can help families or patients access them and listen to a little bit of music before they go to therapy or have a procedure. You can also use other music apps, CDs, or the radio to play music for them.
Touch
Another physiological intervention is touch. Touch therapies have been shown to be noninvasive, nonpharmacological, silent, and very comforting. Comfort Touch is a type of massage developed by Mary Kathleen Rose from Colorado. I worked with her for the comfort touch program that we had at my rehab facility. Comfort Touch is a nurturing, encompassing form of massage that is safe and appropriate for the elderly and the chronically ill. It is adaptable to patients in a bed, a hospital bed chair, a recliner, or a wheelchair. It does not matter where they are and they can remain fully clothed. It is a welcome complement to medical and palliative care measures offered within hospitals, hospice programs, and home care settings. This is something that anyone can do, from CNAs to nurses.
The benefits were amazing, especially on our nursing home side and our long-term ventilator care side. It helps reduce patient's pain, improves relaxation, increases circulation of blood and lymph, and increases flexibility. It provides easier breathing, improved appetite, improved quality of sleep, as well as increased energy and alertness.
We do not have a lot of connection with our families and there is not a lot of touch going on. Think of the patients and residents that do not have family members. Having just this touch therapy is so comforting and healing.
S.C.R.I.B.E.
The tenets of comfort touch are slow, comforting, respectful, into-center, broad, and encompassing. You use both of your hands with broad, full-handed contact, which encompasses the part of the body being touched.
The pressure is directed perpendicularly into the part of the body being touched with particular attention to the amount of pressure to ensure a soothing and calming response. Think of those patients that are so deprived of touch. Comfort Touch can be delivered in any sitting position and any wheelchair bed, chair, massage table, wherever that might be.
Most of these holistic interventions are very simple. It is something that you might just try with yourself and then share with your patient. I have tried aromatherapy and it really helps me to sleep at night and I have tried music, as it is very easy to access. I hope this is something that you might consider, for you, your patients, and your family.
Therapeutic Use of Self
Now let’s talk about you and being therapeutic. Therapeutic use of self is utilizing your presence and your conscious attention to create a healing environment. This includes your verbal and nonverbal communication, the emotional exchange that you have with your patients and families, and other aspects of your personality. That helps when you establish a relationship with that patient that promotes cooperation and healing.
Key Elements of a Therapeutic Relationship
The key elements of a therapeutic relationship include unconditional acceptance, empathy, genuineness, attending and listening, open-ended questions, and silence.
Unconditional Acceptance
Unconditional acceptance should occur regardless of our patient's social standing, ethnicity, background, or presenting illness. We need to treat them the same and use our therapeutic selves to create a relationship with them.
Empathy
We should show empathy. Empathy is not the same as sympathy. Empathy is when we feel with a person, not for a person. Empathy is feeling from the inside outward. It is when we can see with the eyes of another person, listen with their ears, and feel with their heart.
Genuineness
Genuineness cannot really be learned. We need to enter patient rooms and interact with the patients and families with our most clear, genuine, most honest self as we treat them.
Attending and Listening
When you are talking with a patient or their family, especially things like ventilator weaning or trach weaning, it can be scary. It can be very scary for patients when we remove them from their ventilator, cap their trach, or make them walk after they have not walked for three weeks.
One thing to keep in mind when attending and listening is the physical environment. When you are speaking with families and have those special topics to share and want their attention, think about your privacy. Try to minimize interruption so you can get their full attention and they can have yours.
Your posture is important. Anytime you can go into a patient's room and sit down to talk with them it shows them that you are taking extra time with them. Look at them at eye level and lean forward with a relaxed posture and make good eye contact while talking.
Use good listening skills, such as active listening. Show that you are listening, not just putting the breathing treatment in the ventilator or adjusting ventilator settings while they are talking.
Open-Ended Questions
When you are interacting with patients, ask open-ended questions so they can expand on what they would like to share. Try to avoid yes and no questions when you can. One of the strategies of communication is called the reflection strategy. That is when you pick up on the last few words that a patient may say to you and encourage them to talk more about that. You might say, “Could you please expand a little bit more on that point?”
Silence
Silence is important too, as it gives the patient time to think. It also gives the practitioner time to think. Consider that when you are working with patients. Have that moment of silence allowing everyone to get their thoughts in order.
Summary
In summary, the components of anxiety include physiological, emotional, cognitive, and behavioral. Patients and families are both experiencing anxiety as they respond to a perceived threat or danger that is real for them. There are both changeable and non-changeable factors that affect anxiety. Some of the changeable factors are their thoughts or beliefs on what is happening and their arousal by certain interventions. Non-changeable factors include the patient having a history of respiratory disease or already having anxiety. Also, you are not able to change things like their experiences with previous admissions or hospital stays. You can only influence what happens once they hit your doors.
You can use holistic interventions such as aromatherapy, music, guided imagery, and touch therapies. They can be low-cost and effective in managing anxiety. For aromatherapy, there are sprays that are mixed with essential oils, such as jojoba oil, that you could just spritz in the room. You do not need to have a diffuser. You can also take essential oils and put them on a cotton pad. We used to do that and safety pin it to the patient's gown. You always want to check and make sure that there is no aversion or allergies to a particular scent.
Music is very powerful. Have patients think about what music they enjoy. You can help them access that music and encourage the family to participate. Remember the use of guided imagery and the apps for that. Touch therapies, such as Comfort Touch, are easy to learn and are therapeutic. Our patients’ families and caregivers want to do whatever they can to help patients heal and feel more comfortable. They feel so out of control when they are in the hospital with their loved ones. I know I did. I was in a unique situation and I had to help. Comfort Touch is easily learned and effective for managing anxiety and providing comfort.
Also, do not forget about you and the therapeutic use of yourself when you utilize your presence and conscious attention to create a healing environment for your patient and their family.
References
Bae, S. G., & Bae, M. J. (2019). Analysis of health-healing effects according to acoustic signal characteristics in psychoacoustic. International Journal of Engineering Research and Technology, 12(11), 2057-2060.
Bagci, H., & Cinar Yucel, S. (2020). A systematic review of the studies about therapeutic touch after the year of 2000. International Journal of Caring Sciences, 13(1).
Bolzani, A., Rolser, S. M., Kalies, H., Maddocks, M., Rehfuess, E., Hutchinson, A., ... & Bausewein, C. (2017). Cognitive‐emotional interventions for breathlessness in adults with advanced diseases. The Cochrane Database of Systematic Reviews, 2017(6).
Brewer, J. A., Worhunsky, P. D., Gray, J. R., Tang, Y. Y., Weber, J., & Kober, H. (2011). Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences, 108(50), 20254-20259.
Brighton, L. J., Miller, S., Farquhar, M., Booth, S., Yi, D., Gao, W., ... & Maddocks, M. (2019). Holistic services for people with advanced disease and chronic breathlessness: a systematic review and meta-analysis. Thorax, 74(3), 270-281.
Colgin, L. L. (2013). Mechanisms and functions of theta rhythms. Annual review of neuroscience, 36, 295-312.
Davidson, R. J., Kabat-Zinn, J., Schumacher, J., Rosenkranz, M., Muller, D., Santorelli, S. F., ... & Sheridan, J. F. (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic medicine, 65(4), 564-570.
De Sousa, D. P., Hocayen, P. D. A. S., Andrade, L. N., & Andreatini, R. (2015). A systematic review of the anxiolytic-like effects of essential oils in animal models. Molecules, 20(10), 18620-18660.
Dudeney, J., Sharpe, L., Jaffe, A., Jones, E. B., & Hunt, C. (2017). Anxiety in youth with asthma: A meta‐analysis. Pediatric pulmonology, 52(9), 1121-1129.
Fearn, M., Bhar, S., Dunt, D., Ames, D., You, E., & Doyle, C. (2017). Befriending to relieve anxiety and depression associated with chronic obstructive pulmonary disease (COPD): a case report. Clinical gerontologist, 40(3), 207-212.
Freshwater, D. (2002). The therapeutic use of self in nursing. Therapeutic Nursing: Improving Care through Self-awareness and Reflection. Thousand Oaks, CA: Sage, 1-16.
Jacobs, T. L., Epel, E. S., Lin, J., Blackburn, E. H., Wolkowitz, O. M., Bridwell, D. A., ... & Saron, C. D. (2011). Intensive meditation training, immune cell telomerase activity, and psychological mediators. Psychoneuroendocrinology, 36(5), 664-681.
Keville,K., (2009). Aromatherapy a complete guide to the healing art (2nd ed.). Crossing Press
Klainin-Yobas, P., Oo, W. N., Suzanne Yew, P. Y., & Lau, Y. (2015). Effects of relaxation interventions on depression and anxiety among older adults: a systematic review. Aging & mental health, 19(12), 1043-1055.
Lee, Y. J., Choi, S. M., Lee, Y. J., Cho, Y. J., Yoon, H. I., Lee, J. H., ... & Park, J. S. (2017). Clinical impact of depression and anxiety in patients with idiopathic pulmonary fibrosis. PloS one, 12(9), e0184300.
Lee, M. S., Choi, J., Posadzki, P., & Ernst, E. (2012). Aromatherapy for health care: An overview of systematic reviews. Maturitas, 71(3), 257-260.
Li, H. L., He, X. L., Liang, B. M., Zhang, H. P., Wang, Y., & Wang, G. (2015, November). Anxiety but not depression symptoms are associated with greater perceived dyspnea in asthma during bronchoconstriction. Allergy & Asthma Proceedings, 36(6), 447-457.
Lung Health Institute. (2016, Winter). Meditation and its effect on COPD. www.lunginstitute.com. https://lunginstitute.com/blog/meditation-and-its-effects-on-copd/
Mehrabizadeh Honarmand, M., Salehi, M., & Kazemi, N. (2017). The effectiveness of music therapy and relaxation on blood pressure and pulse in the elderly with hypertension. Aging Psychology, 2(4), 293-303.
Moayeri, F., Dunt, D., Hsueh, Y. S., & Doyle, C. (2019). Cost-utility analysis of telephone-based cognitive behavior therapy in chronic obstructive pulmonary disease (COPD) patients with anxiety and depression comorbidities: an application for willingness to accept concept. Expert review of pharmacoeconomics & outcomes research, 19(3), 331-340.
Mogharab, M., Ayoubzadeh, K., & Sharif-zadeh, G. R. (2017). Effect of peppermint aromatherapy on the level of anxiety in patients undergoing colonoscopy. Medical-Surgical Nursing Journal, 6(1).
Ni, C. H., Hou, W. H., Kao, C. C., Chang, M. L., Yu, L. F., Wu, C. C., & Chen, C. (2013). The anxiolytic effect of aromatherapy on patients awaiting ambulatory surgery: a randomized controlled trial. Evidence-Based Complementary and Alternative Medicine, 2013.
Norred, C. L. (2000). Minimizing preoperative anxiety with alternative caring-healing therapies. AORN Journal, 72(5), 838-843.
Panagioti, M., Scott, C., Blakemore, A., & Coventry, P. A. (2014). Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 9, 1289.
Parkes, B. S. (1986). Therapeutic touch as an intervention to reduce anxiety in elderly hospitalized patients. Doctoral Dissertation. University of Texas, Austin.
Smoller, J. W., Pollack, M. H., Otto, M. W., Rosenbaum, J. F., & Kradin, R. L. (1996). Panic anxiety, dyspnea, and respiratory disease. Theoretical and clinical considerations. American Journal of Respiratory and Critical Care Medicine, 154(1), 6-17.
Surani, S., Sharma, M., Middagh, K., Bernal, H., Varon, J., Ratnani, I., ... & Khan, A. (2020). Weaning from mechanical ventilator in a long-term acute care hospital: A retrospective analysis. The Open Respiratory Medicine Journal, 14, 62.
Syeda, S. N., Trucks, E., & Sears, K. (2018). TOPS: Telephonic Outreach in the Pulmonary Service at VA Boston Healthcare System. NEJM Catalyst, 4(5).
Yeh, G. Y., & Horwitz, R. (2017). Integrative medicine for respiratory conditions: asthma and COPD. The Medical clinics of North America, 101(5), 925.
Yeung, J., Couper, K., Ryan, E. G., Gates, S., Hart, N., & Perkins, G. D. (2018). Non-invasive ventilation as a strategy for weaning from invasive mechanical ventilation: a systematic review and Bayesian meta-analysis. Intensive care medicine, 44(12), 2192-2204.
Yohannes, A. M., Kaplan, A., & Hanania, N. A. (2018). Anxiety and depression in chronic obstructive pulmonary disease: recognition and management. Cleve Clin J Med, 85(2 Suppl 1), S11-S18.
Zeidan, F
