Editor’s note: This text-based course is an edited transcript of the webinar, Cultural Awareness and Implicit Bias in Healthcare, presented by Sara Pullen, DPT, MPH.
Learning Outcomes
After this course, participants will be able to:
- Identify the concepts of cultural sensitivity, cultural competence, and cultural humility.
- Describe the need and laws for non-English speaking patients’ rights to a translator.
- Describe health inequity and implicit bias and how it relates to healthcare delivery.
Introduction
Thank you for the introduction. Today, we will be talking about cultural awareness and implicit bias in healthcare. I would like to acknowledge Dr. Remi Onifade, Dr. DeAndrea Bullock, and Dr. Melissa McCune for their contributions to this talk.
Implicit and Explicit Biases Run Through History
Let's start with some implicit and explicit biases throughout history. There is so much we could say about this. One of the most famous examples of this is the Tuskegee Study. The official name of this was the Tuskegee Study of Untreated Syphilis in the Negro Male. It was a study that went from 1932 to 1972 conducted by the Centers for Disease Control and the United States Public Health Service. I will ask you to pause this recording and go to this link as it describes this study in detail. It has only recently come to light precisely what happened. There is also a "New York Times" article called "A Syphilis Study in the U.S. Went Untreated for 40 Years." This is an additional resource. Every time I read about this, it is shocking to me even though I have been aware of it for years.
This was an actual experiment conducted by the U.S. government for 40 years that preyed upon sharecroppers who were the descendants of slaves. They were told that they were being treated for "bad blood" when they were not. They used African-American sharecroppers to see what happens when you do not treat syphilis. For any of you that have seen or treated someone with syphilis, neurosyphilis specifically, it is a terrible way to live and die.
I live in Atlanta and practice physical therapy here. I have patients who are descendants of people from this study. Think about mistrust in healthcare. We are currently seeing a lot of vaccine hesitancy right now. Although the CDC and U.S. Public Health Service have made formal apologies, it is crucial to educate yourself about how implicit and explicit bias and discrimination have been part of our healthcare system for decades.
Culture
Types of Culture
Let's talk about culture (Figure 1).

Figure 1. Atlanta soccer fans on the left and Mexican dancers on the right.
The picture on the left is of fans of Atlanta United soccer. Atlanta is a huge soccer city, and there is a whole culture surrounding soccer. There are costuming, chants, songs, and merchandise. There is also a vast, beautiful stadium. It has culturally taken over the city in many ways. I say this because it is not culture regarding ethnicity, race, language, or country of origin.
On the right, you see two women donned in traditional Mexican dresses in a city parade. This parade celebrates Mexican heritage and culture. I would like you to think about culture not just from one country or race, but also as a city or a sporting culture. Think about this topic more widely.
OK, or 911 Call?
Looking at the pictures in Figure 2, is this ok or require a 911 call?
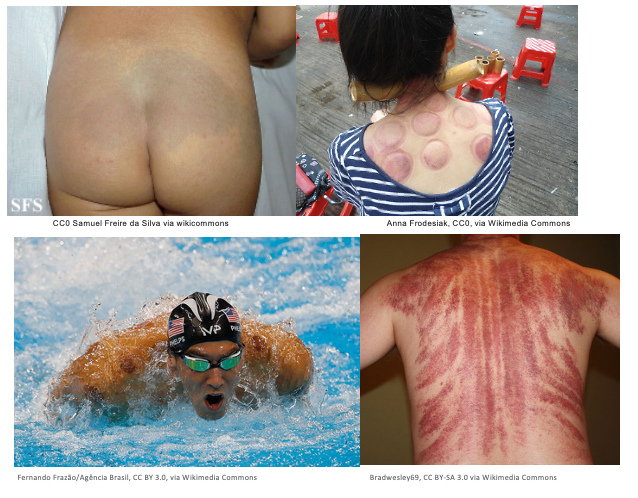
Figure 2. Images of different marks on people.
On the left/top, it looks like a child with a big bruise on their bottom and back. It is not a bruise, but what is called Mongolian spots. They are prevalent in darker pigmented babies. These pigmented areas usually even out by about age three. They are similar to a birthmark but are very specific to darker pigmented babies. There have been cases in the U.S. where babies would be taken away from their families because of these marks. If you see this, you can ask, "I see this mark on your baby's bottom. Can you tell me about this?" In the past, as the comparison was Caucasian skin, these marks were concerning. This is why it is essential to educate ourselves.
Going clockwise to the right, do you know what these marks are on this young woman's back? These marks come from cupping that originated in East Asia. It is a cultural practice of putting a hot jar or cup over someone's skin to pull out everything from impurities, pain, and inflammation. The bottom left picture is Michael Phelps, one of the most excellent swimmers of all time. If you look closely, you can see cupping spots on his shoulders. Did people think Michael Phelps was abused? Probably not. Again, if you see these marks, you can ask about them, but it is not abuse. This is now more in the mainstream of U.S. culture, but it did originate in East Asia.
The bottom right picture shows "coining" and is shocking if you do not know it. Coining involves heating coins and rubbing them down the skin. I have had clients of all cultural backgrounds who have had this done. It originated in South Asian culture. The first time I saw this, I went to my supervisor and said, "I think my patient is being abused." She took a look and identified it as "coining."
I share these with you as we must be aware of different practices of other cultures that we might see. Of course, this is not to say that everyone from South Asia will have this. Additionally, Michael Phelps, a widely known athlete, has used this as part of his pain treatment. In summary, it is seen in different cultural practices and can be very varied and broad. You can always ask them, but it is not for us to jump to conclusions.
How Do We Define Culture?
- a: the customary beliefs, social forms, and material traits of a racial, religious, or social group; also: the characteristic features of everyday existence (such as diversions or a way of life) shared by people in a place or time (popular culture Southern culture)
- b: the set of shared attitudes, values, goals, and practices that characterizes an institution or organization (corporate culture focused on the bottom line)
Merriam Webster
The million-dollar question is, "How do we define culture?" The Merriam-Webster dictionary defines it as "the customary beliefs, social forms, and materials traits of a racial, religious, or social group." Also, culture is the characteristic features of everyday existence, such as diversions or a way of life shared by people in a time or place, like Southern culture). I live in Atlanta, but I am originally from Massachusetts and New England. Many people say "Baby" or "Bless your heart" and serve sweet tea in the Southern culture.
Another definition is the shared set of attitudes, values, goals, and practices that characterize an institution or organization, like corporate culture focused on the bottom line. One of my favorite definitions is from the World Health Organization.
- “Culture should be regarded as the set of distinctive spiritual, material, intellectual and emotional features of a society or a social group, and that encompasses, in addition to art and literature, lifestyles, ways of living together, value systems, traditions, and beliefs.”
- World Health Organization
- This definition stresses that culture is not limited to national, racial, ethnic, or religious affiliation – it is comprised of overt beliefs and practices AND the subtle/ assumed conventions that frame our sense of reality define what is normal and abnormal.
I like this definition of culture as it stresses that culture is not limited to national, racial, ethnic, or religious affiliation. It comprises overt beliefs and practices as well as the subtle and assumed conventions that frame our sense of reality and define what is normal and abnormal to us. Something might be normal to us but not normal to someone else. This is important in healthcare.
Club Culture
- Club Culture...Does It Reflect The Definitions We’ve Discussed? Health Implications?
I am an HIV-focused physical therapist, so I work only with people with HIV and those in underserved communities. Some of my younger patients talk about club culture. Does it reflect the definitions we have discussed? What about health implications? Many that attend nightclubs use drugs or "poppers" to enhance sexual excitement. These include ecstasy or MDMA. This "culture" drug use has significant health implications.
Again, I want you all to think about culture more broadly than just from the standpoint of a country or an ethnic group and how that culture affects our patients' lives.
Definitions
- Cultural Sensitivity
- Knowing that cultural differences and similarities exist and have an effect on values, learning, and behavior
- Expectation that providers show basic empathy and sensitivity to patients in general and treat them in a respectful and caring manner
- Cultural Competence
- The ability to understand, appreciate, and work with people of other belief systems and cultures
- A developmental process and evolves over an extended period.
- Cultural competence continuum
Cultural sensitivity knows that cultural differences and similarities exist and affect values, learning, and behavior. Providers need to show basic empathy and sensitivity to the patients and treat them respectfully and caring manner.
Cultural competence is the ability to understand, appreciate, and work with people of other belief systems and cultures. It is a developmental process that evolves over an extended period. It is sometimes called a cultural competence continuum. I like this as I feel I am in a continuum of understanding different cultures that are not my own. One example is that I had a patient from a different culture. Every time I asked her a question, she would look at her husband, and he would answer for her. I felt it was sexist and could not understand what was going on. However, I could see the look of concern and love in her husband's eyes and knew there was deep respect between the two of them. I realized that I should not judge someone by their culture or anything. My job was to make sure that the information was communicated to my client. It ended up being an excellent relationship between the three of us.
- Cultural Humility
- A lifelong commitment to self-evaluation and critique, to redressing the power imbalances in the physician-patient dynamic, and to developing mutually beneficial and non-paternalistic partnerships with communities on behalf of individuals and defined populations (Tervalon)
Cultural humility is a lifelong commitment to self-evaluation, critique, and redressing power imbalances in physician-patient or provider-patient dynamics. It is better to develop mutually beneficial and non-paternalistic partnerships with communities on behalf of individuals and defined populations. This is by Tervalon. There is a great link (on the slide) from UC Berkeley that includes some great vocabulary on culture.
I like a couple of things about this definition. The lifelong commitment is one. I do not know everything about the culture, my own or other people's. You need to be willing to evaluate and critique yourself or willing to be critiqued by others. For example, one of my students told me that I was mispronouncing her country. She came up after class and told me how to pronounce it. I appreciated that she came up to me as that it was important to her, and it is essential to me as well.
Paternalism does not just mean father, the word's root, but it infers an "I know best" attitude. It is vital to form non-paternalistic partnerships.
Culture Informs:
- How health care information is received
- How rights and protections are exercised
- What is considered to be a health problem
- How symptoms and concerns about the problem are expressed
- Who should provide treatment for the problem
- What type of treatment should be given
U.S. Department of Health and Human Services
Culture informs how healthcare information is received. Think about the example of my client and how rights and protections are exercised. What is considered to be a health problem? I may think something is a huge issue, but in another culture, it might not be. How are symptoms and the concerns about the problem expressed? Who should provide treatment for the problem, and what type of treatment should be given? This is by the U.S. Department of Health and Human Services. There may be some cultures where people do not think respiratory therapists can do a treatment. I have run into this as a P.T. myself.
Cultural Sensitivity & Awareness Checklist
- Communication method: Identify the patient's preferred method of communication. Make necessary arrangements if translators are needed
- Language barriers: Identify potential language barriers (verbal and nonverbal). List possible compensations.
- Cultural identification: Identify the patient's culture. Contact your organization's culturally specific support team for assistance
- Comprehension: Double-check: Does the patient and/or family comprehend the situation at hand? (taking into account family/cultural dynamics of healthcare delivery)
- Beliefs: Identify religious/spiritual beliefs. Make appropriate support contacts
- Trust: Double-check: Does the patient and/or family appear to trust the caregivers? Remember to watch for both verbal and non-verbal cues
- Recovery: Double-check: Does the patient and/or family have misconceptions or unrealistic views about the caregivers, treatment, or recovery process? Make necessary adjustments
- Diet: Address culture-specific dietary considerations
- Assessments: Conduct assessments with cultural sensitivity in mind. Watch for inaccuracies
- Health care provider bias: We have biases and prejudices. Examine and recognize yours
- It’s a fact of life that prejudice and bias exist. Those who deny it are most afflicted! Identifying and recognizing bias will help control its power. To accomplish cultural awareness effectively, health care providers must first: understand her/his own cultural background and explore possible biases or prejudices toward other cultures. Work to overcome these fears, biases, and prejudices and seek help/education to facilitate the process
(Seibert et al., 2002)
I like the Cultural Sensitivity and Awareness Checklist. The first thing to look at is communication. What is your patient's preferred method of communication? You need to make the necessary arrangements if translators are required. We will talk about translators in a minute.
Next, you need to identify potential language barriers, verbal and non-verbal. List possible compensations for this.
You need to identify the patient's culture. You can ask them; do not guess. You can also contact your organization's culturally specific support team for assistance. If you are an inpatient, hopefully, your hospital will have something like this. For outpatient, you may need to do a little more groundwork in your community to find cultural organizations that can assist.
Does the patient and/or family comprehend the situation at hand? It would help if you ensured everyone is on the same page about who you are and your role.
It is essential to identify religious or spiritual beliefs and make appropriate support contacts if needed.
Do the patient and/or family appear to trust the caregivers? That is huge. Remember to watch for both verbal and nonverbal cues.
Does the patient and/or family have misconceptions or unrealistic views about the caregiver's treatment and recovery process? If so, you will need to make the necessary adjustments. This can be anything from asking someone to help you or talking to the patients about making sure you do not have misconceptions about them or them about you.
Are there culturally specific dietary considerations? As respiratory therapists, this is especially important if you are looking at respiratory issues with swallowing or eating.
Conduct assessments with cultural sensitivity in mind, and watch for inaccuracies.
We have biases and prejudices. Those who deny it are most afflicted. You are not doing anyone any favors by saying, "Oh, I do not have any biases," or "I am color blind." We all see it and have it. It is a matter of identifying it. To accomplish this, we must first understand our cultural bias and background and explore cultural biases or prejudices against other cultures. You have to look at yourself and say, "Yeah, that's a problem. Let me make sure that does not come out with my patients." Work to overcome the fears, biases, and prejudices to seek help and education to facilitate the process.
Language
- In 2018, 67.3 million U.S. residents spoke a language other than English at home: this has doubled since 1990 and almost tripled since 1980
- While many people who speak a foreign language also speak English very well, 8% of the U.S. population (25.1 million) is considered limited-English proficient, meaning they speak English less than “very well”
I want you to look at the map in Figure 3 so that you can see the most common non-English languages in the U.S. states. The number one is California, with the most non-English-speaking people.
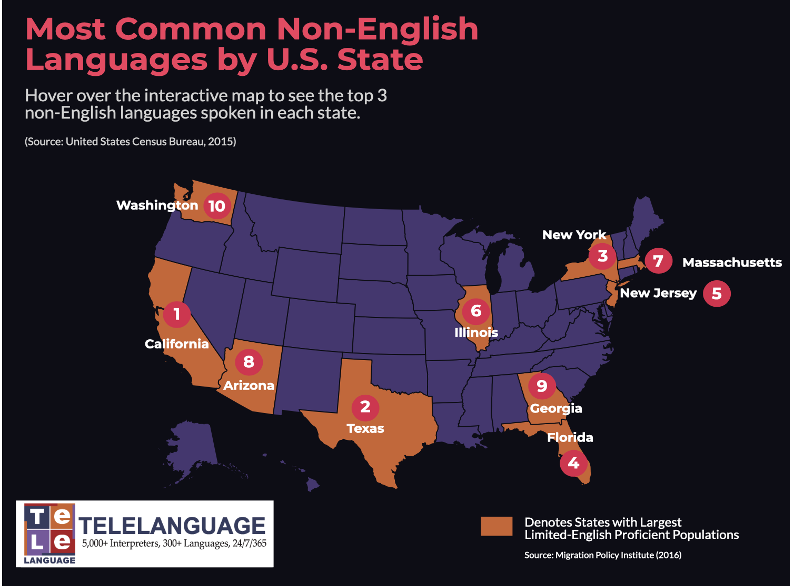
Figure 3. Map of the U.S. with the most non-English languages ranked. Click to enlarge the image.
Texas is next as they are right on the border of Mexico, as well as Arizona. Florida is close to Cuba, and Georgia borders this state. We get a lot of people from Florida going north to New York and New Jersey, which are also very close to Canada. A
In 2018, almost 68 million U.S. residents spoke a language other than English at home. This has doubled since 1990 and nearly tripled since 1980. The number of people speaking languages other than English at home has almost tripled since 1980. Many people who speak a different language at home also speak English very well. However, 8% of the U.S. population is considered limited English proficient, meaning they speak English less than very well.
Civil Rights/Language
We are now going to talk about language and translators as this affects our practices as clinicians.
- 1998: Office for Civil Rights of the Department of Health and Human Services issued a memorandum under Title IV of the Civil Rights Act:
- “The denial or delay of medical care because of language barriers constitutes discrimination and requires that recipients of Medicaid or Medicare funds provide adequate language assistance to patients with limited English proficiency.”
In 1998, the Office for Civil Rights of the Department of Health and Human Services issued a memorandum on Title IV of the Civil Rights Act. It said, "The denial or delay of medical care because of language barriers constitutes discrimination and requires that recipients of Medicaid or Medicare funds to provide adequate language assistance to patients with limited English proficiency."
Let's break that down. Who are recipients of Medicaid or Medicare funds? This is not patients who have Medicaid and Medicare but rather who gets reimbursed by them. This is saying that anyone that gets Medicare and Medicaid reimbursements, basically every healthcare facility, has to provide language assistance, or it is discrimination, under the Civil Rights Act. The only places that may be exempt are private practices that do not accept insurance. Many people and businesses are not in compliance with this.
ACA, Section 1557: Final Update 2016
- So...Hospitals, health plans, clinics, nursing homes, physicians, and other providers must, under federal law, offer “qualified interpreters” to Limited English Proficient patients
- Section 1557 is a “non-discrimination” provision that broadly prohibits discrimination in health care or health coverage based on race, “color,” national origin (including immigration status and English language proficiency). Section 1557 is unique among Federal civil rights laws in that it specifically addresses discrimination in health programs and activities.
There was a final update in 2016 that states that hospitals, health plans, clinics, nursing homes, physicians, and other providers must, under federal law, offer qualified interpreters to limited English proficient patients. They decided that Title IV was a little bit too vague. So in 2016, they said, Section 1557 is a non-discrimination provision "that broadly prohibits discrimination in healthcare or health coverage based on race, color, national origin, including immigration status and English proficiency. It is unique among federal civil rights laws "that specifically address discrimination in health programs and activities."
- 15 states currently provide 3rd party reimbursement through Medicaid and the State Children’s Health Insurance Program for interpreter services (TX = only ASL interpreters)
- Most states with the largest number of non-English speakers do NOT reimburse
- Who is financially responsible for providing interpreter services?
Fifteen states currently provide third-party reimbursement through Medicaid and the State Children's Health Insurance Program for interpreter services. Texas only provides ASL interpreters, but not Spanish interpreters. Do you remember that map? How many Spanish speakers are there in Texas? Remember, there is a big pot of money that states get. And, they can use that pot of money for state services however they want. Unfortunately, the states with the most significant number of non-English speakers do not reimburse for interpreter services.
Who is Responsible?
- All providers who receive federal funds from HHS for the provision of Medicaid/CHIP services are obligated to make language services available to those with Limited English Proficiency (LEP) under Title VI of the Civil Rights Act and Section 504 of the Rehab Act of 1973. However, language interpretation services are not classified as mandatory 1905* services (*coverable, medically necessary)
- States are not required to reimburse providers for the cost of language services, nor are they needed to claim related costs to Medicaid/CHIP, but Medicaid/CHIP providers are still obligated to provide language services to those with LEP and bear the costs for doing so
www.Medicaid.gov
The federal law says, 'You violate federal law if you do not provide interpreters." Still, the state says, "Sorry, we're not going to provide interpreter services." So, who's responsible? The hospitals, the clinics, and the doctors are responsible. Remember, "all providers" who receive federal funds from the Heath and Human Services for the provision of Medicaid or Children's Health Insurance Plan, CHIP services, are obligated to make language services available under the Title IX of the Civil Rights Act and Section 504 of the Rehab Act of 1973. This includes respiratory, speech, P.T., and O.T. However, language interpretation services are not classified as mandatory 905 services, which means coverable and medically necessary. In other words, 905 services are things like surgery. Are you confused? I am as there are many balls in the air.
If you receive federal funds, you have to have translators available, but they are not classified as mandatory under Medicare/Medicaid. States are not required to reimburse providers for the cost of language services or claim-related fees to Medicaid or CHIP. However, Medicaid/CHIP has to provide language services to those with limited English proficiency and bear the cost of doing so. You can go to Medicaid.gov to find this information. It took me a long time to read through this because I kept thinking I was missing something. The truth is that I am missing nothing. If I am a provider (like a hospital), I have to spend my money on interpreter services not to violate the law. Some clinics do not do this as it is expensive. Ultimately, who has to pay? Our patients, who are limited English proficient, pay the price.
Qualified Interpreter
- “Competent Interpreter” “Qualified Interpreter” is defined as an interpreter who “via a remote interpreting service or an on-site appearance.”
- Adheres to generally accepted interpreter ethics principles, including client confidentiality
- Has demonstrated proficiency in speaking and understanding both spoken English and at least one other spoken language
- Is able to interpret effectively, accurately, and impartially, both receptively and expressly, to and from such language(s) and English, using any necessary specialized vocabulary and phraseology
A qualified interpreter is defined as an interpreter who, via remote interpreting service or an on-site appearance, adheres to generally accepted interpreter ethics principles, including client confidentiality, demonstrated proficiency in speaking and understanding, in at least one other spoken language, as well as English. This person interprets effectively, accurately, and impartially with no opinions. They can interpret both receptively and expressively to and from such languages and English, using any necessary specialized vocabulary and phraseology. They need to have interpreter training.
The takeaway is that interpreter services cost money. If your state does not provide state funding, your place of work may be out of compliance with federal law, and the patients will suffer. People die every day from medical interpretation gone wrong.
Language: How Do We Modify Our Clinical Care?
- Options for interpreters:
- Official hospital interpreter
- Language line
- Not speaking English ≠ hard of hearing!
- Shouting does not make someone magically gain English fluency OR hearing ability
- “Ad-hoc interpreters”: family, friends, support staff, strangers in waiting rooms
- What is the risk of using ad-hoc interpreters? Benefit?
As a respiratory therapist, you are often in live or die situations. You need to make sure people and family understand what you say if you do not speak their language. How do we modify our clinical care? An official hospital interpreter is someone that you can call either on a language line, a video call or in person. Language lines can be very frustrating. I have had patients on a ventilator trying to talk through a language line, which is virtually impossible. However, we have to try.
Non-English speaking does not equal hard of hearing. They do not understand English, so stop shouting at them. People, unfortunately, make that mistake all the time. Shouting does not make someone magically gain English fluency or hearing ability.
Ad hoc interpreters are family, friends, support staff, or strangers in waiting rooms. However, there are some risks with using ad hoc interpreters. The person may not be as fluent as you think, or there can be a family dynamic that you are not unaware. What is the benefit? In an emergency, it can be conducive, even life-saving. However, you cannot do it just because you do not want to call the interpreter. This option should only be used in an emergency.
Non-English Speaking Patients
- Patients have the right to a translator
- Make handouts in several languages OR with only images
- Ask for help with translation
- Translating service
- High school/college language professors
- Language graduate students
- Bilingual family members
- Ask for help with translation
- Non-English speakers are less likely to return for follow-up appointments
- Higher rates of drug complications and hospitalizations
- Keep in mind that when using a translator, facts can get lost in translation
https://www.npr.org/sections/health-shots/2014/10/27/358055673/in-the-hospital-a-bad-translation-can-destroy-a-life
Again, patients have a legal right to a translator. You can make handouts in several languages or with only images. Ask for help with translation or provide translating services. In terms of your handouts, you may be able to get assistance from high school or college language professors or graduate students. You have to get them approved by your clinic or hospital, but this would be a great project for someone to do. Bilingual family members or bilingual friends are also great resources. Find someone whose native language is Spanish first. There is always going to be someone that can help with translation for things like handouts. However, you cannot just call anybody into the exam room with you.
Non-English-speakers are less likely to return for follow-up appointments. Higher rates of drug complications and hospitalizations. Keep in mind that when using a translator, facts can get lost in translation. I have provided a link to an NPR article about translators in the hospital, showing how things can go very wrong. Pause this recording and take a moment to read this. Hopefully, this helps you to understand why we need to have translators in our clinics. This article shows that it can be life-saving to have a translator. And, as respiratory therapists, you are in charge of life-saving techniques that a language barrier can severely impact.
Literacy
We all know reading literacy is reading and writing, but what is health literacy?
U.S. Literacy
- 2006: 30 million possess low literacy skills (level 1 or below)
- 2019: 43 million
- Level 1 may be considered functionally illiterate in English: i.e., unable to successfully determine the meaning of sentences, read relatively short texts to locate a single piece of information, or complete simple forms
In 2006, an extensive study showed that 30 million Americans possess low reading literacy at level one or below. Level 1 is considered functionally illiterate in English and unable to successfully determine the meaning of sentences, read short texts, locate a single piece of information, or complete a simple form. In 2019, this number was 43 million, and in 2019, 43 million people. Illiteracy is increasing.
Health Literacy
- Health literacy represents the cognitive and social skills which determine the... ability of individuals to gain access to, understand and use information in ways which promote and maintain good health... health literacy is critical to empowerment.”
Health literacy represents the cognitive and social skills that determine the ability of individuals to gain access to, understand, and use information in ways that promote and maintain good health. Health literacy is critical to empowerment. Who pays for the cost of health literacy? Medicaid and Medicare have the most significant chunk of the burden. For example, people with low health literacy may not know how to take their medication or understand the preventative care they are being told. Thus, they need more medical services.
Helpful Tips
- Ask open-ended questions to assess the patient’s understanding of written materials, including prescription labels.
- Speak more slowly when providing instructions. Be respectful and clear without being patronizing.
- Use graphics and pictures instead of long written instructions
- Use talk back to gauge level of understanding
- Have patients repeat in their own words
Open-ended questions are always the best in terms of assessing patients' health literacy, including prescription labels. "What is hard to understand?" is better than "Do you understand this?" You can also ask, "What is confusing for you?" Or, "Which parts make sense to you?" Speak more slowly when providing instructions. Be respectful and clear without being patronizing. Use graphics and pictures instead of long written instructions. You can use the "talk back" method to gauge the person's level of understanding. The patient repeats the content in their own words. "I want you to take this twice a day, one in the morning before you have breakfast and one in the evening before bed. Tell me when you are going to do this." Have them tell you back. As a physical therapist, I have started to print out exercises with pictures. Then I can write either in English and Spanish, as I am bilingual. If I have a translator, they can write it.
Summary of Literacy Considerations
- Low literacy leads to poor health; 43 million adults struggle with reading tasks
- When creating handouts or disseminating written information:
- Keep it clear, simple, and to the point
- Choose words carefully
- Tell the audience what they need to know
- When possible, make it interactive
- Keep in mind the goal of the information and the goal of the audience
Low literacy leads to poor health. Forty-three million adults struggle with reading tasks. When creating handouts, keep them clear and simple, choose your words carefully, and tell people what they need to know. For example, they may not need to see a ton of anatomical information about the lungs or respiratory system. They may need to know the exercises. When possible, make it interactive. And, keep in mind the goal is to give them X, Y, Z information, and their goal is to do it correctly.
Culturally Sensitive Healthcare
- Healthcare workers must be able to deliver care that is culturally sensitive and is able to meet the needs of an increasingly diverse population
- This is necessary to address continuing disparities in healthcare among certain ethnic and racial groups who still suffer from much higher morbidity and mortality than the rest of the population.
- Culturally competent care has been linked to a better patient-provider relationship, improved communications among patients, families, and healthcare team members, and improved patient outcomes.
Now that we have gone over language and cultural understandings and definitions let's talk about culturally sensitive healthcare. Healthcare workers must deliver care that is culturally sensitive and can meet the needs of an increasingly diverse population. It is necessary to address continuing disparities in healthcare amongst certain ethnic and racial groups who still suffer from higher morbidity and mortality than the rest of the population. Culturally competent care has been linked to better patient-provider relationships, improved communications among families, patients, family members, and members of the healthcare team, and improved patient outcomes. We will go into more detail about that in a few minutes.
- Health care services that are respectful of and responsive to the health beliefs, practices, and cultural and linguistic needs of diverse patients can help bring about positive health outcomes.
- Positive health outcomes = healthy individuals, families, and communities
Culturally sensitive healthcare is healthcare services that are respectful of and responsive to the health beliefs, practices, and cultural and linguistic needs of diverse patients, which can help bring about positive health outcomes. Positive health outcomes lead to healthy individuals, families, and communities, which is the goal.
Implicit/Unconscious Bias
- Implicit associations
- Peanut butter and ________
- Attitudes/stereotypes that affect our understanding actions, and decisions outside of our conscious awareness
- Implicit associations may cause us to have feelings, actions, and involuntary discriminatory practices.
- Affinity bias – tendency to warm to people like ourselves
Let's talk about implicit or unconscious bias. You have probably heard of implicit or unconscious bias. An example of an implicit association is "Peanut butter and..." What do you want to fill in right away? Jelly, right? They go together. These implicit associations are made all the time. Another might be thinking that a racial group consists of "criminals that steal." Or, "They just come to this country because they want to take our jobs." "They are not as strong." "They are lazy." These biases may be buried in our brains and affect our understanding, actions, and decisions, outside of our conscious awareness. Looking back to the peanut butter example, jelly is not the only thing to go with peanut butter, even if I said that it might take a while for your brain to switch gears and say, "Peanut butter and honey," as an example.
Implicit associations cause us to have feelings, actions, and involuntary discriminatory practices. This has been documented in medicine and clinical practice. An affinity bias is an opposite. It is a tendency to warm to people like ourselves and of our ethnicity significantly. While discrimination is undoubtedly an action, affinity bias is as well. This is treating people better because they are of your ethnicity.
This is a shocking study (in the references) about implicit bias in workplace decisions on race. There were two online job sites (Monster and SimplyHired) and two sets of resumes. They had identical resumes with the same schools, job description, previous employment, et cetera. All they did was change the name at the top. The resumes had "white names," like Emily, Anne, Alison, Neil, and Todd, and "African-American names," like Aisha, Keisha, Tamika, Tyrone, and Tremayne. There was a 50% callback gap between both sets of resumes. The people with the "white" names were 50% more likely to be called back for jobs than those with "African-American" names. This showed implicit bias and discriminatory practices.
Can We Work Around Our Implicit Biases?
- Success requires:
- Awareness
- Concern about that bias (motivation)
- Application of strategies to reduce bias
Can we work around our own implicit biases? Success requires awareness and motivation to change. Lastly, it involves the application of strategies to reduce bias. All of these things have to be present.
Essential Elements in Achieving Cultural Competence
- Cultural competence requires that organizations and individuals have the capacity to:
- value diversity
- conduct self-assessment
- manage the dynamics of difference
- acquire and institutionalize cultural knowledge
- adapt to the diversity, and cultural contexts of the individuals and communities served
- Cross et al. (1989); Georgetown National Center for Cultural Competence https://nccc.georgetown.edu
What are some essential elements in achieving cultural competence? Cultural competence requires that organizations and individuals have the capacity to, one, value diversity, two, conduct a self-assessment, three, manage the dynamics of difference, four, acquire an institutionalized cultural knowledge, and five, adapt to diversity, and cultural contexts of the individuals and communities served. If we, as an organization, value diversity, we do not want all of our providers to be of this certain ethnicity. We should actively look to recruit and retain people of different nationalities, cultures, and races.
After a self-assessment, we need to look at our organization to see what is lacking and manage the dynamics of difference. Then, when we have done this, we need to make sure that everyone feels included. Some trainings need to be institutionalized to be a non-discriminatory, zero-tolerance organization. Lastly, we need to adapt to the diversity, and cultural contexts served in your organization.
So, Where Do We Start?
- It doesn’t happen overnight (or in one class) and …We all need support
- Individual self-reflection
- Local community, organization awareness
- Staying aware of policy changes such as:
- Affordable Care Act
- 2020: federal budget cuts
- $4.8 trillion targeting largely Medicaid and the Children’s Health Insurance Program
- HHS cuts (includes NIH and the CDC)
- Vast cuts to H.C. spending
- Food stamps
- Affordable housing
- How will this affect you as a P.T.? (hint: it will!)
Where do we start? This is the million-dollar question. It does not happen overnight in one webinar or one class. We all need support and individual self-reflection, as we talked about on the previous slide. We need to have an awareness of our community and organization. What are the strengths and areas for growth? We need to be aware of policy changes, such as the Affordable Care Act. In 2020, significant federal budget cuts like a $4.8 trillion cut targeted Medicaid and the Children's Health Insurance Program (CHIP). These were cuts for insurance for low-income families and children. It went unnoticed as it was slid between some other legislations. There were also vast cuts to healthcare spending, food stamps, and affordable housing.
How will this affect you as a respiratory therapist? Here is a hint; it will affect all of us. It does not just affect people who have Medicare or Medicaid or people from low-income areas. It affects our entire healthcare system and organization.
Self-Assessment->Reflection->Action
- Given an interaction...
- Assess: Recognize bias within yourself and/or patient
- Reflect: How can I change the next encounter/similar situation? “Gut-checking” à internal process
- How do you reflect on external criticism that you may receive…from patients, co-workers, etc.?
- Emotional Intelligence: take IN information instead of lashing out/putting up a wall if you feel criticized.
- Action: Internal vs. External
- Internal: The reflection itself. Making a plan for” next time(s).”
- External: Acknowledging your own mistakes/room to grow
Self-assessment leads to reflection, which leads to action. This is just like implicit bias. Implicit bias leads to attitudes that lead to discriminatory actions. Let's flip the coin. Assess and recognize bias within yourself, your patient, or your co-worker. Reflect on how you can change the subsequent encounter or similar situation. It is what I like to call a gut-check. What do you feel in your gut? "Oh, I messed that one up. I could do better." This is an internal process. How do you reflect on external criticism that you may receive from patients, co-workers, et cetera? If someone says to you, "Wow, that was offensive." How would you react? Would you get defensive? Would you say, "Oh gosh, you are right. I missed that. Thank you."
Emotional intelligence is taking in information instead of lashing out or putting up a wall if you feel criticized. Let it in, close your eyes, and take a deep breath.
Action can be internal or external. Internal is a reflection and making a plan for next time. External is acknowledging your own mistakes and room to grow. "That was a mistake. I shouldn't have done that." We cannot help our thoughts, but we can retrain them. It is all about catching ourselves.
Health Equity Considerations: COVID-19
- In Memorium:
- George Floyd
- 1973-2020
- COVID-19 survivor
I wanted to wrap up our talk today talking about health equity considerations in the time of COVID-19. George Floyd has become a household name. I always like to pause and reflect that George Floyd was a COVID-19 survivor. George Floyd had and recovered from COVID-19. COVID-19 disproportionally affects underserved and poor communities and African-American Latinx communities. He survived COVID-19 but did not survive racialized violence. His last words were, "I can't breathe." I think of this in terms of COVID-19. Even though we have vaccines, we still see so many disparities in vaccine access in underrepresented minority communities.
- Inequities and social determinants of health that put racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19 include:
- Discrimination can lead to chronic and toxic stress and shapes social and economic factors that put some people from racial and ethnic minority groups at increased risk for COVID-19
- Healthcare access and utilization. People from some racial and ethnic minority groups are more likely to be uninsured than non-Hispanic whites due to factors, such as lack of transportation, child care, or ability to take time off of work; communication and language barriers; cultural differences between patients and providers; and historical and current discrimination in healthcare systems.
Inequities and social determinants of health put racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. Discrimination can lead to chronic and toxic stress and shape social and economic factors that put people from racial and ethnic minority groups at increased risk for COVID-19.
Healthcare access and utilization are other areas of concern. People from some racial and ethnic minority groups are more likely to be uninsured than non-Hispanic whites due to factors such as lack of transportation, childcare, an inability to take time off work, communication and language barriers, cultural differences between patients and providers, and historical and current discrimination in healthcare systems. Think about how we started out talking about the Tuskegee study. That was clear discrimination. People who did not have access to healthcare thought, "The government giving me free healthcare." Things have improved in 2021, but in other ways, they have not.
- Occupation: People from some racial and ethnic minority groups are disproportionately represented in essential work settings such as healthcare facilities, farms, factories, grocery stores, and public transportation: more chances to be exposed to COVID-19 due to several factors, such as close contact with the public or other workers, not being able to work from home, and not having paid sick days
- Educational, income, and wealth gaps: Inequities in access to high-quality education à lower educational attainment à limited future job options àlower paying or less stable jobs (see above)
- Housing: Living in crowded conditions make it more challenging to follow prevention strategies. In some cultures, it is common for family members of many generations to live in one household. Growing and disproportionate unemployment rates for some racial and ethnic minority groups during the COVID-19 pandemic have led to a greater risk of eviction and homelessness or sharing of housing.
People from some racial/ethnic minority groups are disproportionately represented in essential work settings, such as healthcare facilities, farms, factories, grocery stores, and public transportation, where there are more chances for exposure. They may not have paid vacation. Educational income and wealth gaps exist, causing lower-paying or less stable jobs. Housing also can be an issue for pandemic leading to a greater risk of eviction and homelessness or the sharing of housing.
COVID-19: The Great Equalizer?
- The current pandemic is highlighting the health disparities that already exist within our communities
- While COVID-19 places everyone at risk, it has not been “the great equalizer.”
- It will continue to preferentially affect the socially disadvantaged
- Have vaccine rollouts equalized things at all?
- What is YOUR role in addressing health disparities?
When COVID-19 first came on the scene, it was the great equalizer. This is an airborne disease, so everyone should be at equal risk, but actually, it is the opposite. The current pandemic is highlighting the health disparities that already exist within our communities. It places everyone at risk, but it has not been the great equalizer. It will continue to preferentially affect the socially disadvantaged. Have vaccine rollouts equalized things at all? No, they have not, unfortunately, because of things like access to care. What is your role in addressing health disparities? I want you to think about that as we end this presentation. What is your role as a respiratory therapist in addressing implicit bias and health disparities?
Summary
That concludes our talk for today. I want to thank you all for your time. Please feel free to contact me with any questions.
Resources
- Health Literacy: AMA Foundation
- http://www.ama-assn.org/ama/pub/about-ama/ama-foundation/our-programs/public-health/health-literacy-program.shtml
- Ask Me 3 (sponsored by the Partnership for Clear Health Communication at the National Patient Safety Foundation)
- http://www.npsf.org/askme3/
- Health Literacy Studies (Harvard School of Public Health)
- http://www.hsph.harvard.edu/healthliteracy/index.html
- For a complete list of available resources, see http://nnlm.gov/outreach/consumer/hlthlit.html
- HRSA Health Literacy Resources and Course http://www.hrsa.gov/healthliteracy/
- CDC Health Literacy Page http://www.cdc.gov/healthmarketing/healthliteracy/
- National Assessment of Adult Literacy http://nces.ed.gov/naal/
- National Institute for Literacy http://www.nifl.gov/
- Results from the 2003 National Assessment of Adult Literacy http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483
- Health Literacy Assessment Tools (Dept. of Health and Human Services) http://www.ahrq.gov/populations/sahlsatool.htm
References
Andrus, M. R., & Roth, M. T. (2002). Health literacy: A review. Pharmacotherapy, 22(3), 282–302. https://doi.org/10.1592/phco.22.5.282.33191
Aponte J. (2009). Addressing cultural heterogeneity among Hispanic subgroups by using Campinha-Bacote's model of cultural competency. Holistic nursing practice, 23(1), 3–14. https://doi.org/10.1097/01.HNP.0000343203.26216.c9
Bloomfield R. D. (1994). Cultural sensitivity and health care. Journal of the National Medical Association, 86(11), 819–820.
Community Toolbox (n.d.). Enhancing cultural competency. www.ctb.ku.edu. http://ctb.ku.edu/en/dothework/tools_tk_9.htm
Gale, D. (2006). Cultural sensitivity beyond ethnicity: A universal precautions model. Internet Journal of Allied Health Sciences and Practice. https://doi.org/10.46743/1540-580x/2006.1094
Foronda C. L. (2008). A concept analysis of cultural sensitivity. Journal of transcultural nursing : official journal of the Transcultural Nursing Society, 19(3), 207–212. https://doi.org/10.1177/1043659608317093
National Library of Medicine. (n.d.). Health Literacy. www.nnlm.gov. http://nnlm.gov/outreach/consumer/hlthlit.html
Peterson, P. N., Shetterly, S. M., Clarke, C. L., Bekelman, D. B., Chan, P. S., Allen, L. A., Matlock, D. D., Magid, D. J., & Masoudi, F. A. (2011). Health literacy and outcomes among patients with heart failure. JAMA, 305(16), 1695–1701. https://doi.org/10.1001/jama.2011.512
Pignone, M., DeWalt, D. A., Sheridan, S., Berkman, N., & Lohr, K. N. (2005). Interventions to improve health outcomes for patients with low literacy. A systematic review. Journal of general internal medicine, 20(2), 185–192. https://doi.org/10.1111/j.1525-1497.2005.40208.x
Seibert, P. S., Stridh-Igo, P., & Zimmerman, C. G. (2002). A checklist to facilitate cultural awareness and sensitivity. Journal of medical ethics, 28(3), 143–146. https://doi.org/10.1136/jme.28.3.143
Solomon, C. M. (1992, November 2). A world of difference. American Medical News, 27-29.
Stafford JR, Bowman R, Ewing T, Hanna J, Lopez-De Fede A, (1997) Building Cultural Bridges. Bloomington, IN: National Educational Service
Citation
Pullen, S. (2021). Cultural awareness and implicit bias in healthcare. Continued - Respiratory Therapy, Article 114. Available at www.continued.com/respiratory-therapy
