Editor’s note: This text-based course is an edited transcript of the webinar, Ethics in Crisis, presented by Chris Bratton II, JD, L.L.M, and Katie O’Shea, physical therapist, DPT, MBA, GCS, CDP, CCRP.
Learning Outcomes
After this course, participants will be able to:
- Identify the three most common legal documents generally used in clinical care
- Identify approved HIPAA designees
- Identify at least two strategies for re-directing conversations with non-HIPAA identified designees
- Explain the RIPS model framework within clinical scenarios involving end-of-life care and decision making
Poll: Have You Ever Found Yourself in an Ethical Dilemma Involving Direct Patient Care?
We wanted to launch a quick poll and learn more about what type of ethical challenges you all have faced in your clinical practice to feel the audience out and feel the room out and see where things are. It is always interesting to hear the different experiences we see across the nation during these virtual courses—just a larger group of people and see where everyone is coming in. As a treating physical therapist, I am frequently challenged with ethical scenarios. Sometimes they are billing-related, family dynamics-related, physician-driven, or insurance-driven. It is interesting to speak with you all as a respiratory therapist I see daily when in practice. We will give that a little more time. All, almost a split 50-50, we have 60% of folks who have found challenges and about 40% who have not. I want to know where 40% of you guys work and are you hiring?
Poll: Do You Think Ethical Dilemmas Occur More in End-Of-Life Care Than in General Clinical Practice?
In our next poll question, do you think ethical dilemmas occur more in end-of-life than in general clinical practice? End-of-life tends to be more emotions and drama attached, but day to daycare, especially the past 20 months, has sometimes turned into an unfortunate episode of Grey's Anatomy in many hospitals and settings. It is interesting to hear what your thoughts are. About 80% say more dilemmas occur in end-of-life care, about 20% say more in general clinical practice.
Why Talk About Ethics?
Well, there is the apparent licensure requirement. We have to, correct? We are here. Our licenses require it, and we have to talk about ethics. Many factors influence society and culture; pressure from insurance companies and productivity standards go into ethical scenarios. Ethics sometimes become time-sensitive, emotional decisions.
The Ethical Dilemma
Talking about it proactively and not in times of crisis helps us think and find pathways to communicate when those crises end up at our front door. There are absolute rights, and there are absolute wrongs in clinical practice. Medicine comprises individual providers determining the course of treatments, care options, plan of care, and where much is up for interpretation. We have that toolbox of skill sets. How I, as a physical therapist (PT), might treat somebody who had a stroke may look entirely different as another physical therapist that treats someone, These are our toolbox, and this is where the area of gray comes into play, This is where we start to see people making different decisions, acting one way versus the other, and seeing ethics that can be compromised. By definition, according to ethics, these are the moral principles that govern a person's behavior. They comprise professional values ethics, which we will talk about today, and personal ethics. We see this in society, culture, and environmental conditioning. The ethical dilemma arises when our principals get challenged when a choice has to be made between two different courses of action. Sometimes, there is more than one correct answer, especially when looking at those gray areas of clinical practice.
The temptation itself is a dilemma. What kind of personal influence is going on in somebody's life? The areas are gray, and the idea is, is Big Brother watching? Is there a camera in the hallway or the supply room? Maybe I am going on a weekend vacation, and I will take the toothbrush and toothpaste from the supply closet. Where does it start, and what are those gray areas? Our interpretation of ethics is our own value sets. Where do we lie? There is no wrong, but being aware of our interpretation is vital because that carries over into our professional world. Think about the impact of both direct and indirect patient care. If you are not in a clinical role but have questionable ethics or motivating your staff, that can trickle down to the whole team. The influence of society is such a hot topic and divides a conversation point. It has been for quite the past two years almost. We often see patients react differently to providers, or providers react differently to peer-to-peer struggles. Depending on the area of the world or the country you live in, there is undoubtedly a little more of a short fuse in some areas and others, and it can impact decisions made in a very unconscious but biased way.
Then exposure and knowledge, someone who has seen life from a higher 360-degree view has a different perspective. They pull from different areas when making those decisions versus someone starting, has not seen all that there is, and does not understand the bigger picture in this way. Your exposure and knowledge can make an impact on those dilemmas. One thing to remember about these ethical dilemmas, they do not impact one individual or only one metric. They are compound in effect, including the patient, the respiratory therapist, the clinicians, the organization, the healthcare system, and society. We can see that ripple effect on how we see ethical dilemmas unfold.
Respiratory Care Scope of Practice
We will talk through a framework to structure these situations. We want to take a minute to review the scope of practice in Figures 1 and 2. What is an ethics course without seeing your scope of practice up on the screen? The American Association for Respiratory Care position statement goes through where we expect to see our respiratory therapist practice, across the continuum, from neonatal to geriatric.
Figure 1. Respiratory Care of Scope of Practice.
Figure 2. Respiratory Care of Scope of Practice continued.
We see a respiratory therapist in every aspect of care. As a physical therapist, I have worked with many cardiac patients, CHF, COPD. I love respiratory therapists. They help me maximize my patient's function. They help the patient not shut the door and run away because they know I will get them short of breath by moving. I appreciate working with all of you and seeing what you can do in acute care versus outpatient versus rehab settings, rounding out the rest of our respiratory scope of practice. I want to mention that education is a huge component of what you do, but therapists often forget. The respiratory therapists I work with, specifically in the hospital, are busy providing the interventions, treatment, and the education piece sometimes gets trapped.
RIPS Model
- Realm-Individual Process-Situation
- Realm – where the decision is made
- Individual Process – elements of ethical behavior
- Situation – scenario in need of ethical action
- Offers a framework for making ethical decision in a systematic way
- Takes into account various influences on clinicians
The RIPS model is the fancy acronym for the Realm-Individual Process and Situation. The RIPS model is the framework for ethical decision-making. It helps us bring objectivity to a very subjective scenario. The realm is where the decisions are made, the individual process is the elements of the ethical behavior, and the situation is the scenario in need of ethical action. It considers various influences on the clinician, internal and external factors. It might be that the patient is internal and the insurance company is external. Again, it allows us to collect objective data to a very subjective scenario. The realm is the piece of the framework for decisions, focusing on the individual's good, reflecting in most areas the patient. However, the realm can be the clinician or the department manager. It also can focus on the organization and the institution, your hospital, ethics board, and board of directors. It likewise focuses on society as a whole. The mass rollout of vaccines and accessible insurance are excellent examples of society's realm of impact. The individual is the least complex part of the realm, society being the most complex, with intricate and multiple moving parts.
Realm
The realm looks to answer, who is impacted by the problem? Historically looks at if we have experienced this challenge before, and was there a precedent set? Our friends in the legal field use the term "realm" in their cases when they are defending in the courtroom. As clinicians, we look to evidence-based research, randomized controlled trials, and data collection. When we look at evidence-based practice, if an article or journal published in 2021 was a large cohort randomized controlled trial, it is going to be pulling data from 2018 or 2019. The evidence-based research we look at will always have a lag. The realm forces us to look at active cases in our health system and how we have handled this before. When we look at individual examples, this might be writing refusals for patient's treatment and using your time doing something non-clinical.
As a physical therapist, if the respiratory therapist comes to the door and I am about to get started, that respiratory treatment is going to enable my therapy treatment to be better, but it is going to throw off my whole schedule because now I am in the room, and I need to leave. For a therapist, this might change how we schedule or how we have to see other patients. You may have therapists tempted to write a note for that session when they should not be. However, you focus on the patient who needs respiratory therapy treatment for optimal care.
When we look at organizational examples of the realm, looking at productivity expectations, we see those changes frequently based on insurance, which is an example of organization. Layoffs are another example of the realm of organization and pay cuts. With all the changes in staffing that we have seen over the past two years, and areas that impacted ourselves, our job, the patients, the care they have access to, and the care they receive while in the institution, it is our societal realm. Looking at healthcare reform, vaccine mandates, accessibility to care, and healthcare literacy levels. What kind of healthcare is available in underserved areas versus privileged areas. We look at all areas of the realm where the decision is made.
Individual Process
We quantify ethical behavior in four ways: moral sensitivity, moral judgment, moral motivation, and moral courage. Sensitivity is recognizing and being aware. It is perhaps saying I am aware, and I need to be mindful of what I think might not be okay. It is familiar, and it is no judgment. It is awareness. Moral judgment is where we objectively find the difference between right and wrong. Moral motivation looks at what other components are included in the ethical decision. Are there personal or financial gains to be made? We see professional areas impacted by personal thoughts and vice versa. If you have someone who may be struggling to pay their bills in their personal life and professionally, there is an opportunity for them to pick up over time, see extra patients for bonuses, it starts to create a very gray area of what you are willing to be motivated by for that patient and/or clinical practice. Moral courage is having the courage to go against a popular decision. Asking yourself and saying, hey, this is not okay, we need to act differently.
Situation
We look at the RIPS situation piece and identify a scenario that needs action. Choice A or choice B. It looks at distress, an issue that identifies if the decision is unable to be made, and maybe that is a decision you can make at your level or needs to go up the chain of command. Temptation, looking at those secondary gains, being honest and objective about what they could be. Are there additional gains that I need to look at? In the situation part of the RIPS framework, we look at patient compliance, patient refusals, clocking in, clocking out, that ability to manipulate the time clock to an eight-minute rule, clocking outright at that eight-minute mark, and then getting your full 15 minutes.
Applying the RIPS Model
- Step 1
- Recognize and define the ethical issues
- Step 2
- Reflect
- Step 3
- Decide the thing to do
- Step 4
- Implement, evaluate, re-assess
We identify those areas of the RIPS model, the realm, the individual process, and the framework that makeup step one, recognizing defining issues. Step two is now reflecting on all the information you gathered from step one. Step three, deciding the wrong thing to do, is usually pretty straightforward. The right thing to do is tricky because there are two correct answers, and you usually need additional support and recommendations from peers to make a decision. Step four is implementing that decision, evaluating its success, and then reassessing if you keep going with that decision or if something else is needed.
As a brief background, I am an attorney, but I am not a typical attorney that you would think of in the traditional sense. From my perspective, we are not coming at this from an area of being a plaintiff's attorney or defendant's attorney concerning some malpractice suit that is not where we come from, rather we focus on planning, and a big part of that is healthcare advocacy and helping our client through that continuum of care. Whether we are setting up their estate planning documents or helping them transition. If they are at home, maybe they need in-home care, assisted living to skilled care. We are helping them through that entire transition. We are not expecting you to get into the weeds of this to figure out all the intricate details of their estate planning documents, what they need and what they do not need, but it is also suitable for you to know in casual conversation because you probably spend much time talking to these patients. Maybe they are missing something. Maybe they do not have a healthcare power of attorney in place, a HIPAA, or a living will. If you can spot an issue and say you may want to talk to somebody about it, it is always a good idea because you add value to that client. That is where we are coming from, our perspective in this process.
Legal Documents
We certainly want our clients to have their legal documents in place. At least their basic ones, financial power of attorney, healthcare power of attorney, living will, and HIPAA documents. There is a difference in what is required in the law to execute certain documents. A higher level of capacity is required to execute a power of attorney than to execute a will. We have to assess whether our clients have the requisite capacity to execute these documents. If they do not, then what are our options?
Will
- Executor
- Funeral Representative
- Beneficiary
- Purpose is to distribute assets of the decedent
- But…
- Joint Accounts
- Beneficiary Designation
- Operation of Law
We will go over some of the basic documents. A Will is a document that passes along assets to the heirs. Now, this may be done via trust, but for our purposes, we are going to focus on the Will being the document that passes along assets to the heirs. An executor is named, meaning who will handle the estate if the person passes away. There will be beneficiaries, individuals receiving the inheritance underneath the Will directed to that beneficiary or another route such as a trust how assets are distributed. There are also other ways that assets can pass outside of probate because you have to go through the probate process when you have a Will.
Power of Attorney (POA)
- Financial Powers
- Immediate or Springing
- Durable
- General or Special
- Multiple Agents
- Revocable
If you own an account jointly with another person, like your 401k or 403b, your IRAs, annuities, or own a piece of real estate with another person as joint tenants with rights of survivorship, all of these types of accounts and ownership types will pass outside of probate. The will does not control in those situations. We want to make sure our clients have a financial power of attorney who can handle the affairs for our clients if they become incapacitated, whether for a short period or an extended period, like if they have cognitive decline. Is it going to be an immediate power of attorney or springing power of attorney, immediate means as soon as the principal signs the document, the document is in effect, the agent can do whatever the principal can do. If it is springing, it is not effective until two doctors certify that the principle's incapacitated that it becomes effective. You will probably not be looking at the financial power of attorney or maybe even the healthcare power of attorney at times, but these are the different types. You will often hear a power of attorney referred to as a general durable power of attorney. Durable means that it survives incapacity. It is effective when the person is incapacitated. General means that it is broad in scope versus a special POA.
For instance, I am buying a piece of real estate, but when the closing occurs I will be on vacation. I can give Katie a special POA to sell that property on that specific day related to that property. Once the end of that day occurs, that power of attorney is no longer in effect. We can have multiple agents under a financial power of attorney, meaning more than one person can act or make it that they have to act in concert. These documents are revocable at any point in time by the principal, assuming that the person has the requisite capacity to revoke the documents.
Health Care Documents
In a healthcare document, you will hear the term advanced directive, an umbrella term. We have a living will and healthcare power of attorney, the healthcare power of attorney being the proxy directive, and the living will be the instructive directive. I am sure everyone is well aware of a living will versus a healthcare power of attorney. The healthcare power of attorney, and remember that both documents do not take any powers away from the principle. They give powers to another person, the agent under that specific power of attorney.
A healthcare power of attorney is operative when it is transmitted to the physician. Now the physician must determine whether that patient has the mental capacity to make their own healthcare decisions or not. If the physician feels that they do not have that capacity, they will turn to the agent to make healthcare decisions. If the patient has the requisite mental capacity, they will always make their own healthcare decision. Now, different states have different laws concerning the appointment of agents under certain documents. I am in New Jersey but also licensed in Pennsylvania, and these two states are very close to one another; even between these two states, there are different laws.
Guardianship Law
- New Jersey Court Rules 4:86 et seq.
- New Jersey Statutes 3B:12-1 et seq.
- Major revisions enacted January 11, 2006
Some states will allow multiple agents to be appointed under a healthcare power of attorney, and some states do not want multiple agents appointed. Some states will have next of kin laws, while others do not. I believe four states do not have next of kin laws, New Jersey being one of them. Meaning if there is no healthcare power of attorney in place by statute, can the medical provider turn to someone next of kin for direction regarding healthcare treatment. New Jersey is not one of those states, but they have a next of kin law by statute next door to Pennsylvania.
Guardianships
- Involuntary court supervised decision maker
- Incapacitated person cannot manage own affairs
- Cannot execute documents
- New law deletes all reference to “incompetent”
- Replaces with “incapacitated or alleged incapacitate” (AIP)
If our clients do not have the requisite capacity to execute documents, we are forced into a guardianship position, meaning the court will deem the person incapacitated and appoint someone to manage their affairs, both of the person and the estate, a court proceeding. Someone has to petition the court, where the judge will write an order saying that this person is incapacitated and cannot handle their affairs. We refer to this individual as the alleged incapacitated person.
Privacy Issues
- NEW law provides that physicians and psychologists may disclose medical information in affidavits/certifications supporting guardianship applications
- No breach of privacy
- N.J.S. 3B:12-24.1(d)
Indeed, we have HIPAA issues that we have to address. However, in New Jersey, there is, and I am sure every state has its law, that physician psychologists can disclose medical information by affidavit and certification supporting the guardianship application without violating any HIPAA rules.
Who May Be Guardian?
- Spouse or domestic partner if
- Living with incapacitated person (or would be if not for nursing home placement)
- Heirs or friends
- Office of the Public Guardian – age 60 or over
- Any other proper person
- Consideration is given to surrogate decision-makers chosen by incapacitated person before incapacity
- 3B:12-25
The court will look through a hierarchy level regarding who can be a guardian. Usually, the court will look to the spouse first. If there is a spouse, typically the spouse will be named the guardian if they are the ones applying, and then maybe they will look to the children, grandchildren, siblings, kind of goes in order. We also have an Office of Public Guardian that may step in if no family is in place, but the court will typically consider that hierarchy level.
Determination of Need for Guardianship Services
- New law specifically outlines different types of guardians (N.J.S. 3B:12-24.)
- Outlines powers and duties
- General Guardian
- Limited Guardian
- Pendente lite; Temporary Guardian
- Outlined by order
There are different types of guardianship. We can have a general guardianship, limited guardianship, or a temporary guardian. All of this will be outlined by order. The order will let whoever may be looking at it, whether you are a medical provider or administrative staff in the hospital or other setting that you may be in. They will see who the guardian is and what powers they have. With the general guardianship, the guardian controls all aspects of that incapacitated person's life concerning personal decisions, healthcare decisions, financial decisions. They control everything. A limited guardian, perhaps the incapacitated person, can do certain things. Can they determine where they live or whom they associate with? Can they be involved with some of their healthcare decisions? Can they be involved in some of their financial decisions? It is all outlined in the guardianship action and the guardianship order.
Critical Need or Risk of Substantial Harm
- Physical or Mental Health or Safety and well-being in jeopardy
- Property or business affairs may be repossessed, wasted or misappropriated, dissipated, lost, damaged, or diminished, or not appropriately managed
- In best interest of alleged incapacitated person
It could be an emergency medical guardianship. If there is a substantial risk of harm or some critical need where the person's health is in danger or the wasting of an estate is in danger, then there could be an emergent guardianship in place. Indeed, if the individual's physical health or mental health is in jeopardy, the courts can step in and appoint someone temporarily to make those decisions. Also, maybe the person who runs a business or has a particular property that they do not want to be wasted or misappropriated, the court may step in and appoint someone to handle those affairs. They are always looking to determine the best interest of that alleged incapacitated person.
Trust
- Types
- Revocable vs. Irrevocable
- Varying purposes
We briefly spoke on this previously when we were talking about a will. There are many different types of trusts, and sometimes clients will come into the office, and they will say, I need to trust. We try to dig a little deeper. Why do you feel that you need to trust? My neighbor has a trust, or my cousin's friend has a trust, so I need a trust. However, that may not be the case, and we use a trust for different purposes; it can be revocable or irrevocable. We can use them for tax planning and asset protection planning purposes for probate avoidance. In some states, it is very cumbersome and expensive to go through probate, and in those states, you do not want to go through the probate process. A revocable trust will avoid that. Alternatively, if you have a property in multiple states, we may not want to go through probate in multiple states. A trust may avoid that, but it depends. A trust will determine where assets go. Again, we will focus on a will for this webinar being the primary vehicle for the disposition of assets to beneficiaries. I always love hearing about guardianship, and I know we have talked about this before, but back when Netflix put out the show, I Care, painted such a different picture for folks of what guardianship is. It helps to clarify it in some way. We want to apply this to the RIPS framework we talked about, creating that realm, that individual process, the situation, and applying it to the legal documents.
RIPS in Action with Legal Documents
- Unauthorized representatives trying to make decisions, direct care, direct finances
- Step 1
- Recognize and define the ethical issues
- Potential financial gains
- Patient’s advanced wishes not being followed
- Recognize and define the ethical issues
- Step 2
- Reflect
- Impact of family guilt and other psychosocial considerations
- RIPS in Action with Legal Documents
- Reflect
- Step 1
- Unauthorized representatives trying to make decisions, direct care, direct finances
- Step 3
- Decide the thing to do
- Ethics committee
- Decide the thing to do
- Step 4
- Implement, evaluate, re-assess
- Care conference
- Implement, evaluate, re-assess
- Step 3
We are looking at unauthorized representatives trying to make decisions, direct care, and direct finances. Step one will be recognizing defining ethical issues and applying that RIPS framework looking at the realm. People, the individual's risk of exploitation, concern wishes are not being followed. The institution piece of the realm will be looking at the hospital or the healthcare agency. Are they liable if the patient has taken advantage of when they are deemed under stress or lack mental capacity? HIPAA is a federal regulation, but there is now a lack of trust for that agency when there are breaches. How does this impact the organization? The individual process. Looking at our moral sensitivity, moral judgment, and moral courage, what are we seeing impacted there, Pretty much a and wrong scenario where there is a correct answer and that is wrong in following the legal documents available. And then, the situation part of step one is looking at distress, both the patient and the caregivers—a high emotion time when looking at that information. Then also the temptation to take advantage of maybe inheritance funds that are coming available that were not previously available.
Once you have gathered all that information in step one, step two reflects on it. Family guilt may become involved here. There might be other psychosocial considerations. Family members who were not present may be coming out of the woodwork.
We hear that term a lot. We are reflecting on all the other variables going into this decision-making. Then we look to step three. It is deciding the thing to do. The legal document piece is a little more black and white because those documents are in place that we heard Chris talk about. That is very much you have to follow those documents. When you get into situations such as Chris elaborated on guardianship, things of that nature, folks who are found unknown, , found down outside with no identification, no one claiming them, or homeless population, then things have to go up that chain of command, the Ethics Committee. looking at that, that is where step three is deciding the thing to do and using your chain of command to find the things to do. And then step four, this is probably the area when we are looking at legal documents that, in this case, applying the upstream part is significantly cut and dry. You apply the outcome and then move forward—reassessing if different legal documents are brought to the table later.
HIPAA
- Acronym stands for the Health Insurance Portability and Accountability Act, a US law designed to provide privacy standards to protect patients' medical records and other health information provided to health plans, doctors, hospitals and other health care providers, developed by the Department of Health and Human Services.
Those of you reading may never run across an issue where you have to determine, know whom you are taking direction from, or listen to concerning the course of care when the family gets involved. However, that being said, we work with many medical providers, many facilities. We hear stories of family members coming in, trying to give their two cents about the type of care that should be provided and the course of treatment. Moreover, you have to be cognizant of whom you disclose information to and whom you are taking direction from. You cannot let yourself be put into a position where a loud family member is bullying you into a situation where you are disclosing information or taking direction from someone you should not be taking direction from or someone you should not be disclosing information to. If you need to push it up to your chain of command, then you push it up, and you let someone else make that decision, but do not let yourself be influenced by someone who is simply trying to bully you or trying to be loud enough to get you to do something you should not be doing. This falls within the HIPAA realm, and it falls within that other document we discussed, that healthcare power of attorney, that proxy directive of who can decide if the patient cannot make their own decision. everyone on here is well aware of the HIPAA laws, Health Insurance Portability, and Accountability Act. Again, this is a federal law designed to provide specific standards to protect patients' medical records and other healthcare information concerning any information that can identify that person.
Summary of HIPAA Privacy Rule
- A major goal of the Privacy Rule is to assure that individuals’ health information is properly protected while allowing the flow of health information needed to provide and promote high-quality health care and to protect the public's health and well-being.
- The Rule strikes a balance that permits important uses of information while protecting the privacy of people who seek care and healing.
- HIPAA Representative
The primary goal of this is to protect the client's healthcare information while striking a balance where medical providers can disclose and share certain information.
Pre-emption of State Law
- The bill supersedes state laws, except where the Secretary determines that the State law is necessary to prevent fraud and abuse, to ensure appropriate State regulation of insurance or health plans, address controlled substances, or for other purposes.
It is a federal law. Any federal law will preempt state law unless there is a situation where state law is necessary to prevent some fraud or abuse or ensure some other appropriate state regulation.
SEC.261. Purpose
- It is the purpose of this subtitle to improve the Medicare program under title XVIII of the Social Security Act, the Medicaid program under title XIX of such Act, and the efficiency and effectiveness of the health care system, by encouraging the development of a health information system through the establishment of standards and requirements for the electronic transmission of certain health information.
The purpose of this was to improve the Medicare and the Medicaid program under the Social Security Act and the efficiency and effectiveness of the healthcare system in disclosing information, sharing information, and making sure there are standards in place to protect patient information.
SEC.1171. Definitions
- HEALTH CARE CLEARINGHOUSE – A public or private entity that processes or facilitates the processing of nonstandard data elements of health information into standard data elements
- HEALTH CARE PROVIDER – Includes a provider of services (as defined in section 1861(u)), a provider of medical or other health services (as defined in section 1861(s)), and any other person furnishing health care services or supplies
We want to focus on the healthcare provider. A healthcare provider provides some medical or other healthcare services or furnishes healthcare services or supplies. We want to understand that the HIPAA regulations govern all healthcare providers.
What Information is Protected
- The Privacy Rule protects all "individually identifiable health information"
The Privacy Rule protects all individually identifiable healthcare information, and it is not identifiable information. It is anything that could lead to the identification of that individual. We will get into some examples a little bit later.
SEC. 1171 Definitions
- INDIVIDUALLY IDENTIFIABLE HEALTH INFORMATION – Any information, including demographic information collected from an individual, that:
- is created or received by a health care provider, health plan, employer, public health authority, life insurer, school or university, or health care clearinghouse; and
- relates to the past, present, or future physical or mental health or condition of an individual, the provision of health care to an individual, or the past, present, or future payment for the provision of health care to an individual, and:
- identifies the individual; or
- with respect to which there is a reasonable basis to believe that the information can be used to identify the individual
This definition under Section 1171 is any information including demographic information that is created or received by a healthcare provider, health plan employer that relates to the past, present, future physical or mental health of the individual, condition of the individual, or provision of payment for that individual, and that identifies the person or lead to the identification of the person.
Who is Covered by the Privacy Rule
- Applies to health plans, health care clearinghouses, and to any health care provider who transmits health information in electronic form
- Health Plans
- Individual and group plans that provide or pay the cost of medical care are covered entities
- Health Care Providers
- Every health care provider, regardless of size, who electronically transmits health information in connection with certain transactions, is a covered entity
HIPAA covers all healthcare providers. We want to make sure that everybody is listening. If you are providing care, you are covered by HIPAA regulations.
Required Disclosures
- A covered entity must disclose protected health information in only two situations:
- to individuals (or their personal representatives) specifically when they request access to
- Health and Human Services (HHS)
There are certain required disclosures. You have to give information to the individual if they are asking for their healthcare information or if there is a power of attorney in place that you feel is a valid power of attorney. You can rely on that document to disclose protected healthcare information and then to HHS.
Permitted Uses and Disclosures
- A covered entity is permitted, but not required, to use and disclose protected health information, without an individual’s authorization, for the following purposes or situations:
- To the individual
- Treatment, Payment, Health Care Operations
- Uses and Disclosures with Opportunity to Agree or Object. Where the individual is incapacitated, in an emergency situation, or not available, covered entities generally may make such uses and disclosures, if in the exercise of their professional judgment, the use or disclosure is determined to be in the best interests of the individual.
- Facility Directories
- Directory of patient contact information
- A covered health care provider may rely on an individual’s informal permission to list in its facility directory the individual’s name, general condition, religious affiliation, and location in the provider’s facility
- The provider may then disclose the individual’s condition and location in the facility to anyone asking for the individual by name, and also may disclose religious affiliation to clergy
- Facility Directories
There are certain instances where the covered entity is permitted but not required to disclose certain information. If the individual is incapacitated in an emergency, the covered entities can make specific uses and disclosures if it is in the individual's best interest to exercise their professional judgment.
Other Provisions
If you are in an emergent situation and feel it is in the patient's best interest, you can disclose certain information. Hospitals usually keep a directory of patient contact information concerning facility directories. If someone calls in and asks explicitly for that patient by name, you are allowed to say whether they are there or not and whether they are, for instance, stable or not, you cannot give specific information regarding their healthcare information, in any case. A personal representative can treat an agent under a power of attorney the same as the principal. You can disclose the information unless you have some knowledge, for instance, maybe a power of attorney has been revoked, or you feel there is some kind of fraud. Other than that, you are safe in releasing protected healthcare information to the agent under a power of attorney.
Safeguards
- Each person described in section 1172(a) who maintains or transmits health information shall maintain reasonable and appropriate administrative, technical, and physical safeguards—
- To ensure the integrity and confidentiality of the information;
- To protect against any reasonably anticipated –
- threats or hazards to the security or integrity of the information; and
- unauthorized uses or disclosures of the information; and
- Otherwise to ensure compliance with this part by the officers and employees of such person
Every person, who transmits healthcare information has to maintain reasonable and appropriate administrative safeguards.
Penalties
The bill imposes civil money penalties and prison for certain violations. We do need to take this seriously. There are civil penalties and criminal penalties that can be imposed for certain violations. There are two sections under which someone can be charged for a HIPAA violation, 1176 and 1177. 1176 is a general failure to comply with the required standards.
SEC. 1176. General Penalty for Failure to Comply with Requirements and Standards
- SEC. 1176 (b) LIMITATIONS-
- OFFENSES OTHERWISE PUNISHABLE– A penalty may not be imposed under subsection (a) with respect to an act if the act constitutes an offense punishable under section 1177
- NONCOMPLIANCE NOT DISCOVERED – A penalty may not be imposed under subsection (a) with respect to a provision of this part if it is established to the satisfaction of the Secretary that the person liable for the penalty did not know, and by exercising reasonable diligence would not have known, that such person violated the provision
If you are not complying with HIPAA, you can be charged under 1176. In general, the penalty will not be imposed if it is established to the satisfaction of the secretary that the person liable for the penalty did not know and, by exercising reasonable diligence, would not have known that the person violated the provision
Civil Money Penalties
The penalty (Figure 3) can be anywhere from $100 to $50,000 per violation up to a calendar cap of $1.5 million. These are steep penalties. It is not the person violating the HIPAA regulations but also their employer. An employer has to make sure that all the compliance is in place.
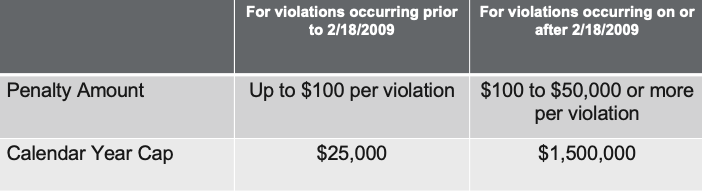
Figure 3. Civil Money Penalties.
SEC. 1177 Wrongful Disclosure of Individually Identifiable Health Information
- SEC. 1177. (a) OFFENSE – A person who knowingly and in violation of this part
- Uses or causes to be used a unique health identifier
- Obtains individually identifiable health information relating to an individual or discloses individually identifiable health information to another person, shall be punished as provided in subsection (b)
- SEC. 1177. (b) PENALTIES – A person described ins subsection (a) shall
- Be fined not more than $50,000, imprisoned not more than 1 year, or both
- If the offense is committed under false pretenses, be fined not more than $100,000, imprisoned not more than 5 years, or both, and if the offense is committed with intent to sell, transfer, or use individually identifiable health information for commercial advantage, personal gain, or malicious harm, be fined not more than $250,000, imprisoned not more than 10 years, or both.
We have SEC. 1177, which is a wrongful disclosure of protected healthcare information. Types of individuals punished under 1177 would be anyone who knowingly violates HIPAA, uses the information or obtains it for some financial gain, or discloses it to another individual for financial gain. The fine can be $50,000 and imprisonment of a year. If the offense is committed under pretenses, the fine is $100,000 and imprisonment of five years, or if the offense is committed with the intent to sell, transfer or use the identifiable healthcare information for commercial gain, then you are looking at a $250,000 fine with up to a ten-year penalty for imprisonment.
HIPAA Notice
Every covered entity has to provide notice of its practices concerning HIPAA. The notice has to describe how the covered entity uses and discloses protected healthcare information and what that covered entity's duties are to protect that person's privacy. They also have to give notice on how the individual can complain if they feel that there is a violation of HIPAA, they can complain to HHS, and it has to include some point of contact for further information and if that person wants to file a complaint that covered entity.
Confidentiality
When we are talking about confidentiality, everyone has to speak to their healthcare provider confidentially, and you must make sure that that person's healthcare information is kept confidential. Any data or information that leads to that person, identifying that person and whether its course of treatment, current condition, payment for particular treatment plan-no matter what it is, that person has the right to maintain confidentiality, and you have to maintain that confidentiality for that patient.
Don’t Assume
The HIPAA Privacy Rule should not be read to create barriers to normal communications with a patient's family or friends. The rules permit doctors or other health care practitioners to share information directly relevant to the involvement of a spouse, family members, friends, or other people identified by a patient. If the patient has the capacity to make health care decisions, the doctor may discuss this information with the family, or others present if the patient agrees or, when given the opportunity, does not object. Even when the patient is not present, or it is not practical to ask the patient's permission because of emergency or incapacity, a doctor may share this information with family members or friends when, in exercising professional judgment, the doctor determines that doing would be in the best interest of the patient.
We do not want to assume anything. Going back to whom you can speak to, you cannot assume that you can speak to anyone. We do not know the backstory. Someone can come in and say they are married, but how do you know? How do you know they are not estranged? How do you know that it is not an abusive relationship or that children are involved? Maybe mom is not doing well with their health condition, and maybe they want inheritance. They are trying to find out more information and dictate mom's course of treatment. You do not want to assume that you can speak to specific individuals. If your patient is there and they indicate to you, whether in writing or verbally, that you can disclose information, you can undoubtedly disclose that information. If you have a room full of people and the patient says yes, you can disclose information. While again, we do not want to assume that we can disclose to certain people because we do not know.
Reporting
Sometimes practitioners are required to disclose certain information. Certain infectious diseases, HIV, tuberculosis, have to be reported to state and local public healthcare agencies. If you see any signs of mistreatment or abuse, you must report that information to protective services. If you suspect that the patient's condition inhibits their ability to drive and potentially harm other individuals on the road, you should report that information to the DMV. I think clinically, we often see in our hospitals and rehab settings that this family number "A" is there with the patient and then family member "B" comes in, and it becomes this explosive firework situation. It is like watching a daytime soap opera unfold in your life, and you do not know whether to change the channel or get popcorn. I think it is essential for clinicians to hear that, to know that you are protected by the federal laws that we learned about to say and answer those documentations. Sometimes because of the loudest person, we want to make the situation better, make it go away, or appease them. Go to your supervisor if you do not want to take on that responsibility. Many medical providers at certain levels should not do that. Let the supervisor make the call.
RIPS in Action with HIPAA
When we talk about applying the RIPS framework to our HIPAA portion of this, we are looking at unauthorized representatives attempting to find out information on a patient using threats and legal retaliation. How much do we love when families come in and say, "I will call the news station. You do not know who I am?" We will use this example to take that situation and deescalate it.
- Situation: Unauthorized representatives attempting to find out information on a patient, with use of threats and legal retaliation
- Step 1
- Recognize and define the ethical issues
- Patient privacy
- Patient’s preferential choice at a time when they were fully aware
- Recognize and define the ethical issues
- Step 1
We are looking at the realm. The individual will be the patient they are trying to find healthcare information on. The institution will be at play in this because they are responsible for upholding the patient's and their HIPAA and privacy. Society is a tricky piece of representative action with HIPAA because the societal piece will not come into play unless there is a true breach and that breach is made public, which is a real scenario that genuinely can happen. Looking at it from the framework is a hypothetical scenario that is not in the current moment. The realm is going to apply to the individual and the institution. You are looking to obtain the facts. Are there documents, are there designated, care providers? Who are the stakeholders involved? The patient, the clinician, the family members, other staff members in the hospital, the institution. We are looking at the consequence of the decision and the impact on that more extensive level.
What a respiratory therapist may disclose by trying to appease from a customer service standpoint could significantly affect the organization in terms of liability of those HIPAA guidelines and the fines. Looking at our policy and procedure manual and our code of ethics, these are things that we kind of, policy and procedure manual, you break out on orientation day and then it goes on a shelf. You review our code of ethics when your licensure renewal comes around. However, these documents are there to support you in your clinical practice. When you are in these scenarios and in that heightened awareness, or heightened situation, you go to those documents. The individual process of the HIPAA scenario will look at the moral sensitivity, recognizing again, there is, being aware that it is probably an uncomfortable conversation. First of all, there is probably someone agitated and taking the tone that they should not be with you. It is being aware of the situation and looking at the judgment. In this scenario, there is a wrong in disclosing and not disclosing information, what is protected and what is not. Looking at the motivation as this comes into play many times.
Clinically, there is usually a secondary gain when family members come in very upset. They are trying to make up for the lost time, financial gains on the table, and sibling rivalries. I find the moral motivation in the HIPAA piece to be a strong and crucial component. The moral courage, knowing you have your manager's support, you have a whole institution behind you who wants to do the thing, you will be supported. Taking yourself out of that situation, getting yourself out of the room where the family member is distraught. The situation created in this kind of scenario is distressing, and there is an ethical dilemma because it is a wrong choice to be made.
Once we have established all of step one, look at the patient's privacy, and if someone has advanced documents in place. What were their choices at a time when they were fully aware? As clinicians, this is where we get caught up because we work with a patient one-on-one. Maybe we are in there giving them breathing treatments two-three times a day, you start to form a rapport with the patient. They may be saying things differently from the documents they signed them five-ten years ago, which puts you as a clinician in a challenging situation because all of a sudden, you have a family member who is not the designee asking you for information. You have "Mary" who has told you things and disclosed things that make you believe there might be more going on here. As our clinical role, this is not where we are to disclose that information. We will look at the patient's choices when they are fully aware. We all know medications have side effects on cognition; delirium is an actual thing at the hospital. The patient may be saying one thing but not aware they are saying it. Later down the line, once everything is back to a status quo in their life, there can be repercussions for that disclosure.
- Step 2
- Reflect
- What factors may be impacting these actions?
- Money? Insurance? Power? Retaliation? Guilt? Greed?
- Reflect
We reflect on the hypothetical and less objective. What factors might be impacting these actions, family dynamics, trying to be the hero, sibling rivalry? Alternatively, is it money, insurance, power, retaliation, guilt, or greed?
You get into some heavy things here by reflecting on all which can be at play. The framework is excellent because when you have situations that come up, it is easy to go down the rabbit hole of your thoughts and your interpretation of that family member's angle that does not belong in the objective data collecting sense. It belongs in step two, where you can bring that to the table, put it out there and then move forward.
- Step 3
- Decide the thing to do
- Federal regulation makes the choice incredibly clear
- Make appropriate supervisors aware
- Decide the thing to do
The HIPAA scenario is the easiest because federal regulations make a choice explicitly clear. You have your supervisors aware of the situation who can support you in those acts and follow up the decision.
- Step 4
- Implement, evaluate, re-assess
- Notify legal representatives of attempt by unauthorized representatives
- Our duty is not to fix the family dynamics, but we do have a responsibility to inform legal parties
- Offer options for added security when speaking with a legal representative if concerned about false identification
- Implement, evaluate, re-assess
Our duty is not to fix the family dynamics, but we have a responsibility to inform legal parties. Notify legal representatives of an attempt by an authorized representative, putting into place other safeguards that can be made on the account, whether that looks like a separate password or a "break the glass" where you have to double sign into a chart to access that information, to force folks to take that second timeout before they proceed—looking at all those pieces in the HIPAA framework. Redirecting that conversation with non-HIPAA-identified designees can be very challenging. The first step will always be to ask for providing those documents. As a clinician providing that one-on-one care, this is something that your first line of defense will be to bump up the chain to your manager. Whether it is your respiratory therapy manager, the nursing floor manager, or the unit manager clinical specialist, you have many folks to pick from within healthcare systems and institutions. If you are more of a satellite center, you have the executive director usually for that facility. If you feel comfortable, you can ask for those documents to be brought in, start that conversation, then inform the manager.
Being proactive in these conversations is immense, setting expectations and referring back to the federal regulations. These are not rules that hospital A is doing one way, the outpatient satellite center is doing the second way, and the pulmonary function lab down the street is doing a third way. Everyone has to follow the HIPAA guidelines federal regulation HIPAA guidelines. It is being very clear-cut and direct. When this comes up, I have said to patients and patients' family members, "Have you ever been to a physician where you have to sign that HIPPA release?" They say, "Yes, and roll their eyes, " That is when I know I can connect to them and say, "Hey, we also have to file that here in this institution. I understand it is a pain, but unfortunately, I cannot give you that information. Here is our HIPAA disclosure." It is evident in black and white.
We often get swamped in our day-to-day practice in answering calls, going to rapid responses, which becomes a "hamster wheel" of getting our checklist items done. When we try to take a moment and validate someone's feelings, we see that people often need to be heard. We are not looking to fix the situation but acknowledging where that person is. "I see you are upset, and I am sorry for that frustration you have to go through now. I know I will not answer your problem today, but I feel for you as a human. I see you are struggling, and I am here." I say this with caution because when you do this to somebody who is already in a heightened state, there is a high likelihood you are going to get that emotional dump dropped back onto you. Be aware, have an exit strategy in place for yourself. There are times when I have found it beneficial to allow that person to have that emotional dump because then it has allowed me to move forward in my care plan in a different way.
Then there are other times it has backfired. It is a trial and error, but it is certainly a strategy that does help in validating where someone is. Letting someone know they are heard and seen will give you closure. Providing a contact level for your supervisory compliance center next level chain of command that a person knows they have someone they can go to and speak to additionally. It does help provide information, support, and reassurance to these families in the middle of these family dynamic turf wars. I cannot imagine that the medical provider will get reprimanded for not disclosing the protected healthcare information of a patient without proper proof. However, I can almost promise you that you will get reprimanded if you provide information to someone you are not supposed to provide information for, and then that patient makes a complaint. We need to err on the side of caution. If you do not have proper proof, do not provide that information to that individual unless you know that they have the ability or consent from the patient. Likewise, please put it back onto your manager, "I understand I need proper proof, I can give you information, that these are the guidelines that we have to follow, I can speak to my manager," and you can give them the manager's information. I would rather see everyone err on caution rather than disclosing information because the person is "loud." The first time that happens as a clinician versus experienced in life makes a difference, but it does not make it sting any less.
One of our employees had a situation where her daughter was in college, and the daughter was in an accident. One of her friends called her mom because the daughter was unable to call herself. The mom called the hospital where she was, and they would not provide her with any information. You can say you are the mom or dad, but if that person is 18 or older, they are an adult. If you have a child going off to college, you cannot get healthcare information if you are not an authorized representative under HIPAA. They are an adult, and you are not entitled to that information.
Ethical Challenges with end-of-life Decision Makers
Ethical Challenges with End-of-Life Decision Makers
- Lack of plan
- Guilt
- Anger
- Grief
- Unresolved Trauma
- Fear
- Family Dynamics
- Secondary Gains
We are going to talk about ethical challenges with end-of-life decision-makers. Hospice is sometimes a scary word, both families and providers like to shy away from it, but it is a part of life, and how fortunate are we if we can make that journey a little more comfortable for people. I have been a physical therapist for 15 years and have worked in acute care, rehab, home care, outpatient. I have seen palliative services in the hospital and home care setting and hospice services. I cannot say that end-of-life care is what I want to do all day, every day, but when it is something that I am involved in, I think it is a privilege to be part of. One of my favorite clinical areas of practice is in the hospital. That is why I currently practice per diem. It is incredible how you get thrown into situations as a clinician, whether you are a physical therapist, respiratory therapist, occupational therapist (OT), or nursing colleague. Situations happen quickly, and you may be without an option at that moment.
We want to talk through challenges with end-of-life decision-makers, starting with emotions. It starts with a lack of a plan, leading to these heavy emotions.
As clinicians, we make a care plan for what we are doing with our patients and our goals. It keeps us on track and allows us to reassess. If we do not have that plan, we tend to fall into paralysis or analysis paralysis, getting input from everyone, which I think is a bit worse because everyone has an opinion. We have not had those conversations when we think about that end-of-life decision. As a patient, I am forced to think about my lifespan and the impact of all my loved ones, family members, friends, and my world- considerable information to take in and process. Has anyone ever tried to put paint swatches up in their house, and when people come over and ask, "What do you think?" By the time five people have looked at it, you are thinking, "I am not going to paint because this is too much pressure." The lack of plan and getting input from everyone else makes the decision even cloudier than it already is. Here we talk about planning, having those conversations, and those documents, which allow for a plan or that initial conversation. When we do not have those things in place, we start to see guilt, a lot of the "I should have done," and remorse starts to come to the table, which is hard. You cannot see the current situation. You are looking at the situation, trying to make amends vs. what is happening in front of the family.
Guilt can change our emotions and change our perspective. As clinicians, when we are talking to those family members, they do not hear our recommendations or hear options. They focus on the need to be with loved ones 24/7 because they were not there before. Anger is another emotion that we experience in end-of-life decision-making. It is undoubtedly part of the stages of grief that we will talk about next. It is a place where we see families and our patients going through, and it masks other feelings. You will get the loudest person in the room, the non-compliant or difficult patient. Correlating anger is fear—many folks mask other feelings and are unwilling to listen.
Then we look at grief as a whole. We have five stages of grief. We have denial, anger, bargaining, depression, and acceptance. When we look at the end-of-life, we sometimes do not have the time to process those emotions. Looking at where someone is and the potential to be, sometimes end-of-life decision-making is minute by minute. We are not even talking hospice in six months. We are talking about critical moments left. You are not going to have someone who can process through those stages. As clinicians, what type of feedback and verbal and nonverbal skills can we bring to the table to help someone be open and aware and make the best decision to help their healing and recovery. A big piece of end-of-life decision-making is unresolved trauma, regret, making amends, harboring resentment, not providing forgiveness, or folks wanting to keep someone alive to try to get forgiveness they have not sought out prior to this point. It can make folks do many different things. We might stand at the nurse's station saying, "What is going on?"-this is unhealthy. The reality is that this family member, this individual, does not know how to cope in any other way. I think of a patient who moved from out of state to the current state because they were trying to make amends with a family member. Their family member then dropped dead, unfortunately. Regrettably, they had a massive heart attack about 20 days after they had moved up. That patient was there. My patient was there and witnessed all with their family member. Then they collapsed, had a panic attack-type of thing, came into the hospital. It was an interesting situation because this person was stuck in a depression phase of their grief and could not move. They literally could not move due to unresolved trauma. Every time we tried to mobilize during a therapy session, it would result in tears and emotions labile personality. The entirely independent person in their early 30s suddenly required four people to stand up without a physical reason for it. We see the effects of that unresolved trauma, and that individual always kept saying, "I am doing it for my mom because I could not make it better when she was here." Those are heavy things when they happen in our clinical practice.
When you are with a patient finishing a breathing treatment, the mask is off their face, and you may not know what will be said to you. Think about those things and be prepared for them. Telling someone, "Yes, you are hurting, I hear you and it is okay to feel this," goes a long way. Fear is a massive piece of what stops folks from evaluating hospice on the patient and the family. I am sure many of you have come across families where they are the power of attorney of someone who is cognitively impaired, and they do not want their loved one to know that their terminal diagnosis is terminal. They withhold information, but they are the power of attorney and are allowed. Fear of losing someone, that fear of death is not something many people embrace, and it is heavy. Helping folks be aware is a considerable barrier to end-of-life decision-makers. Secondary gains, insurance policies, inheritance can make some end-of-life decisions not great. They are expediting things quicker than what would naturally happen because someone is trying to get a payout on a policy. Be mindful that even with all the legal documents in place, end-of-life care does come with high and sometimes volatile emotions. While providing grief counseling is outside the respiratory scope of practice, education, disease process, discharge planning, and case management is within the scope of practice of respiratory therapy.
As clinicians, we can speak to our knowledge and understanding of the expectations to help a family member make a better-informed decision. If working with a client with end-stage COPD, end-stage CHF, they will have respiratory challenges in simple exertional tasks. Helping to understand those expectations can help someone hear it another time. We need to hear something seven times to sink in and click. Also, it helps the medical team have that conversation. Palliative and hospice services provide staff trained to help manage those emotions and help manage the grief process while that patient is living and once they have passed. They are great resources and ways to console when you have those end-of-life decision-making skills. As a physical therapist, I am very fortunate when asked for opinions, but I will always ask for a palliative care consult. I feel fortunate that I can bring that conversation to the table and make end-of-life care less damaging than it sometimes is as the time-sensitive motion nature of end-of-life care. Be conscious of times we can plan, and sometimes it is in the moment, and we do not have that opportunity to plan.
Engaging the Decision Makers
How are we going to honor the end-of-life wishes? The 5 Wishes is a proactive document allowing patients to plan for and say what they want in their end-of-life care. As respiratory therapists, we are not completing this with the patient, but we can direct them towards this document available on the internet. There is a great website, and it allows people to start to have that conversation, even during the process of doing your advanced directives. I am in my 30s and can tell you it was a weird process to complete an advanced directive because you are not thinking about end-of-life at that point. I am grateful not to be considering that. However, spelling out what you do and do not want is emotional. Helping families to understand is part of the process, starting the conversation on what we are looking to do with our end-of-life care and taking the crisis out of things. We are trying to put a plan where there is no plan. Quality of life is different for everybody. It might be looking at a tree with a cup of coffee, on a catamaran looking at dolphins, or it might be on their couch watching QVC. None of our quality of life is wrong. We need to help families understand the difference between their perception and the patient's perception.
In the case study, we talk about a patient with end-stage lung cancer. The patient was genuinely ready to pass on, and the wife was not ready to allow that to happen. It was the quality of life that was such a different perspective. The family member is looking at it from, "You can get a trach, be on a portable vent, and you will be alive." While the patient was actively dying, dyspneic, and wanted to pass. The patient's quality of life was entirely different from the family member's. Support from the interdisciplinary team is a large part of the decision-making process. Healthcare as a system is a little bit broken. We tend to think more in silos. As a physical therapist, I think in my silo. We all are in our silos, occupational therapy, nursing, physicians, respiratory therapy, or theology colleagues. Our insurance is set up in silos, but leaning on our team members is a big piece of end-of-life care.
As a physical therapist, I offer options from ability, endurance, energy conservation, pulmonary hygiene, even home and outpatient settings. A large piece of that is in the Respiratory Practice Act that you are doing in the acute care setting. If a patient is discharged on home care, respiratory therapy may not be going out to that house. As a physical therapist, I can support what they have learned and pulmonary hygiene in auscultation. It is in my scope of practice, and I can help with that. If we have a severely compromised patient with their cardio home function, and walking is not an option for them, I am the part of the team that will help look at wheelchair mobility. Is it power or manual? Do we need to look at the hospital better? Those are things I bring to the table. My occupational therapy counterparts focus on their daily living activities, their ability to do self-care, and their dignity with their ADLs. One of the most challenging points for folks as they get into end-of-life care is the need for personal care completed for them. An example, wiping themselves is a personal issue. Occupational therapists can use adaptive equipment to help somebody learn and keep that dignity, which is an incredible piece of what we offer to the table. That may be the difference between someone going to a long-term care center or inpatient hospice versus someone being able to go home and take care of themselves at a bed-bound level.
For many of the members of the team, we do not have time to talk throughout today, but many folks are completing their plan of care as part of the interdisciplinary team - nursing, physicians, spiritual, pastoral care staff all rely on one another as we are looking at those end-of-life decisions and bringing purpose to the moment.
Many times death is terminal. There is an endpoint or end objective when we talk about end-of-life. However, helping folks to find value and purpose as they are transitioning brings much comfort to folks and brings much comfort to families and the decision-makers. We do not start that conversation, but things come up naturally in conversation. When those moments come up, feel empowered to go and explore them and ask more questions about them. An example that comes to mind is a patient who was a Holocaust survivor and was now end-of-life. The family was not in the country, and she was initially by herself. She had stories she never told her family because it was too emotional for her to get through. She wanted to pass it on and be shared. It came up in one of our therapy sessions while taking a rest break in our mobility. As a physical therapist, I knew that it is not, productivity-wise, what I am paid for in the hospital. My manager does not want to hear I am helping a person write a memoir. However, I know we have a great patient advocacy department that will go and sit with patients. I made one quick phone call, and the patient advocate was able to come to the patient's room and dictate notes for them. She put a memoir together, and she found purpose in that. Do not be afraid to go down that conversation or discussion when these moments come up.
Re-Directing Conversations
Some conversations do require redirection. When we have those conversations, we talk about our own value set, withholding biases. It is okay that we have them. Being aware of those biases is essential, is how we change and make movement if we choose to. Reviewing HIPAA laws, any federal regulations, or state practice acts that apply to where you are practicing, you have to follow those laws, or if not, you will be in orange jumpsuits paying fines. I see clinicians shying away from having conversations or promising things that will never happen because it cannot come from a federal standpoint. However, it is okay to use that when trying to redirect the conversation—providing opportunities for the additional documents to be presented. Do they have the wills, power of attorney, or advanced directives? Ask for the information to be brought to the table and provide opportunities for questions and answers. Inform your manager that someone will need to be involved at a level higher than me. Many times, this is not a conversation that should fall on you as a sole clinician. We talked earlier about implementing EMR safeguards. Breaking the glass, we have to sign in twice, and passwords are placed on protected accounts.
I had a family member who would call in and say who they were and knew the date of birth to get information. The person was listed as a power of attorney. They were allowed to receive information. We found out they were calling and pretending to be the sister to gain information which became an issue. We had to put a password on the account. When the person would call in, they had to give a password before a physician or another medical provider would talk to them. There are additional ways to implement safeguards and go from there.
Personal Ethics
When we look at engaging decision-makers and having these conversations, we look at our values, what we stand by as ourselves, and who we are as a person? We are not looking to change that when we interact with our patients. Being aware is beautiful. I will be vulnerable. I am not a cat person, primarily because of allergies. However, I would adopt more dogs if my dog was not mean to everyone. For me, that is a value. However, some folks are cat people and do not understand dog people. Maybe I will not bring up that conversation with a patient because I know it is a piece of myself that will not change. Every culture and religious belief has different thoughts on the afterlife and what happens. Especially in end-of-life, some people may want to talk about it. It might be an area you are not comfortable with or know anything about.
Maybe it is an area you are interested in learning more about and can say, "I do not know, but I would like to hear what is going on in your life or what your thoughts are." Indeed, some religious beliefs do preclude some medical care. I am sure many of you have worked with Jehovah's Witnesses who refuse blood transfusions. I have seen patients pass away because they will not receive blood products. It does not matter whether there is an opinion or not. It is their belief and value. Understanding my value may not line up with that, or it may, but supporting someone where they are within their ethics. Stress is a huge piece when looking at ethics and high emotional conversations. What is our threshold to take on the emotional dump of others?
Sometimes we do not even think about it. Suppose my car broke down this morning. I spilled coffee on my scrubs, and my dog vomited on the way out the door. My stress might have already been high coming into work. In comparison, my colleague's coffee showed up at his door this morning. His car was warmed up for him when he got in the car. His morning was stellar. His stress level is even lower because he had a fabulous morning, where I am still cleaning my coffee off of me. Our ability to have stressful conversations is already from a different perspective. Understanding where we are in our personal life impacts our professional life. I do not think this is rocket science. It is all common sense. We lose sight of these things in day-to-day practice, being aware of where we are in our stress response. Personal ethics the perception of quality is probably entirely different in quality for each person. It is okay, but understand it will not look the same. If you have a poor parent caregiver relationship, you might find it challenging to understand a healthy family dynamic. Families at the bedside are distraught over someone in that end-of-life phase, and it might not make sense to you. Your reactions might be guarded and cold because it is your perception of where you come from in your life. You are not looking to change it, but have an awareness.
We see death with dignity laws passed in California, Colorado, DC, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, and Washington, allowing competent adult clients to decide to end their lives with medical assistants. It is a topic of conversation. It took pro-life pro-choice that we see in the fetal stage and applied to the adult stage. I have worked in companies where we did this, and while I have never personally been involved with it, I know the procedure manual had a piece that spoke to exempting employees who disagreed with the death of dignity laws. We will see that evolve much more depending on where these laws go in the future. The takeaway from this line, what we have a tendency towards in our personal lives can carry over to our professional life, and that is okay. We are not changing ourselves. If we acknowledge it, we can be aware and more mindful of it.
Challenges of Bedside Care
- Staff burn-out
- Over capacity institution
- Understaffed shifts
- Resource availability
- Institution and Community
- Operational pressures
- Length of stay
Let's look at the real challenges of bedside care and staff burnout. Healthcare has always been a bit of a challenge. I think the past 20 months have raised that challenge, leveled up but not in a good way. Staff burnout is vast. We see institutions at 110% capacity. We see beds in the ER, out into the hallways, and consistently understaffed shifts. We see nurses forced to work at higher than is safe assignment values and respiratory therapists covering an entire hospital. It is challenging to cover patients in a smaller hospital or three different floors, let alone an actual emergent issue where you are part of the response team. We see the effects of consistency in understaffed shifts, resource limitations, availability in the institutions, availability of equipment post-discharge, and community resources. Home care providers have two to three weeks of delays to take on patients coming out of the health system, rehab center, or hospital setting. We are seeing patients. We see non-compliance higher than ever.
We see that the revolving door of readmission is higher than ever because patients are not managed as well as before. It is not a high benchmark because there were many re-hospitalizations prior to COVID. Operational pressures and length of stay has and always will be a benchmark for care, regrettably. Pushing discharge will always be a piece we see in the health system. It seems that we see the length of stay being pushed on to us more than ever. Insurance changes in home health during the beginning of 2020 entirely changed how patients received care and how many visits they were allotted. It changed that whole scope of practice and the continuum of care. While it stopped fraud in the areas it needed, it also limited care to patients reliant on the system. Also, in 2022, changes were slotted for what patients can access in their outpatient setting for therapy, a whole another area of cost containment and service reduction. The insurance challenges will impact our bedside care, as we see our patients coming back in sicker and sicker because they are not getting the care they need.
On Labor Day, a family member was in the hospital and had a heart attack and is doing fine now. I baked for this individual and stopped because they changed to low sodium heart-healthy diet. I was not going to enable it. The family member said to me at Thanksgiving, "Why do not you bake for me anymore, you do not love me?" I was unwilling to be compliant. I accepted it was something I could not do anymore. My family member refuses to comply with those things and uses more guilt to get sweets out of somebody because I will not do it. They are ordering them from the grocery store, or when their private duty caregiver comes in, they are having them bring them snacks. We see this a lot with our diabetic population. The non-compliance piece is a huge challenge. Then the families who take to "Dr. Google," go down their path of what they think is appropriate and do not follow medical direction because it is not something they accept. We are treating more western medicine, and maybe they are doing more eastern medicine, and the two are not aware of what is going on. Certainly, withholding information is a huge piece when discussing end-of-life care and patient care in general. It all impacts transparency and what options we even have to bring to the table. We are going through all these things, be kind to yourself in your clinical practice. All the variables are at play for you, the patients, and caregivers. How can we make the best decisions as we provide that information?
Case Study #1- Goals of Care
- You are called to the bedside while the PT/OT is attempting to treat this patient. Due to desaturations while moving the head of bed from 45 degrees to 90 degrees, her O2 needs are increasing.
- At rest, Shelly is producing copious amounts of serosanguinous secretions, dyspneic, tachypneic, and requiring 6L O2 via nasal cannula maintaining SpO2 only at 87%.
- Patient is refusing yankauer for oral secretions which have increased dramatically with 45 degree change in head of bed position.
For the next section, we talk through a couple of case studies and apply some of the knowledge we discussed today. I will read through this first case here, and then we will use the RIPS and talk it through. Shelley is a 58-year-old female with end-stage lung cancer. She came into the ER with increasing dyspnea, increasing O2 needs at home. She was on two liters of oxygen, now requiring four.
- Therapy refuses to attempt further mobility due to patient’s physiologic function.
- Patient is screaming she wants to die and does not want further care; however, is listed as full code.
- Patient’s partner is screaming she does not want her to die and begging for patient to accept suction, meds, and treatment.
- Medical team is at bedside attempting to discuss goals of care.
She is disengaged during her hospital stay, refusing meds, labs, meals, not working with therapy. The medical team had arranged for Shelley's partner to be present for a therapy session at noon to help mobilize Shelly and get her out of bed. They thought this would encourage participation. The therapists elevated her head of the bed from 45 degrees to 90 degrees sitting up, and her oxygen needs increasing. You, the respiratory therapist, are called to the bedside while PT/OT attempts to treat the patient. At rest, Shelley's producing copious amounts of serosanguineous secretions. She is dyspneic, tachypneic, and now requires six liters of oxygen while only maintaining a pulse ox reading of 87%. She is refusing to use a yankauer but is using nasal suction. Secretions have increased dramatically with the 45-degree change in their head of bed position. Therapy refuses to attempt further mobility because of her physiologic response. The patient screams that she wants to die and does not want further care. She is a full code. The patient's partner is screaming that she does not want her to die and begging the patient to accept suction, meds, and treatment. The medical team is at the bedside attempting to discuss goals of care.
- MD orders a nebulizer for patient comfort and asks you to provide the treatment to the patient. When applying the facemask, Shelly swats it away and attempts to keep pulling it off her face.
- Shelly’s partner is POA and demanding continued medical intervention. Shelly continues to refuse intervention and has no advanced directives however is conscious and coherent.
- What should happen next?
The physician orders a nebulizer treatment and asks you to provide the treatment to the patient as the respiratory therapist. When applying the face mask, Shelly is swatting at you and attempts to keep pulling it off her face. Shelley's partner is a power of attorney and demanding continuing medical intervention. However, Shelly refuses the intervention and has no advanced directive, conscious and coherent.
- What is the Realm?
- What is the Individual Process?
- What is the Situation?
What should happen next? Our next step should be looking at the RIPS and applying our steps. The first step, the realm, is the individual. Shelly is our primary focus of this care. We are seeing her goals, she is cognitive and competent, and she wants to refuse care. The individual process, moral sensitivity, recognizes and interprets an ethical situation. The patient's wishes clash with the power of attorney's wishes—the moral judgment hypothetical piece. Shelly is decompensating, and she is actively sick. What happens if Shelly cannot communicate knowing she previously did not want these interventions? However, her power of attorney is not respecting her wishes. We do not know the moral motivation in this situation and the moral courage. At this point in the case, there is no need to step up and go against a popular decision or implement an action yet.
In this situation, we have a medical diagnosis of end-stage lung cancer with a clinical presentation that could be consistent with the act of dying process. Conversations need to be had regarding Shelley's wishes while she is capable. Step two is recognizing. As we reflect on this scenario, we do not have time on our side. We have to make a quicker decision during active decompensation, and the medical team forces that conversation. Step three, looking at deciding the thing to do, the care goals, and rule-based decisions. Shelley is competent and being able to make those decisions for herself. Looking at who else may need to be involved in these decisions, the attending, what of the medical staff, is there an Ethics Committee conversation. And then step four would be implementing and monitoring the patient's status. with this scenario, this case ended with the patient transferring to the ICU for further medical management. The ICU Attending can talk about comfort measures while Shelley is cognitively competent to say what she wants. The morphine push was started, and about 12 hours later, Shelly did pass.
The names changed for HIPAA compliance, but this was a volatile and emotional case where therapy happened to be in the room doing family training, and things did not go well. Despite the patient not wanting treatment, respiratory therapy was put in place to provide treatment. We are looking at what needs to be done and who needs to be involved. The medical team decided to have further conversations about comfort care and end-of-life. The reality for that patient was that the partner was very against the word hospice. Finding a different way to talk about comfort care and not hospice allowed that transition to happen.
Advocating for Your Patient
- What is Elder Law
- How can they help?
- Legal
- Asset Protection
- Estate Planning Documents
- Trustee
- Medicaid
- Elder Care Coordination (ECCs)
- Health Care Advocacy
Let's briefly talk about your ability to advocate for your patient. There is a slight difference between elder law practice and life care planning practice. Typically with an elder law firm, they may engage in estate planning, asset protection, filing Medicaid applications if necessary, assisting clients with making certain decisions regarding their Medicare or the Medicare supplement. The difference in being a life care planning law firm is that elder care coordination (ECCs) is in place, helping our clients with their healthcare advocacy. They are our elder care coordinators, and they are the ones that help our clients through that continuum of care as life changes in health conditions. Examples include health deterioration, needing help to obtain home services, visiting physicians, or prescriptions delivered to their homes. They take different forms. Our staff has a registered nurse, a social worker, a colleague with a Master's in counseling, and a colleague with a background in AAL, and they are all certified dementia practitioners who offer much support to the family and the clients themselves.
How can we help the family get through this continuum process in conjunction with our elder care coordinators? Whether it is in document preparation, asset protection, trust preparation, Medicaid applications, making sure the clients are protected, and everyone enjoys the remainder of their lives however they want to live it. If whatever area you are in, if you see something with a client that may be lacking, maybe they do not have a healthcare power of attorney in place or a living will or a HIPPA release or any of those types of things that you may see in general conversation that is lacking, maybe point them to a life care planning law firm or an elder law firm depending on ultimately what their needs are.
End-of-life Care Planning
Ideally, we want this to be proactive. We want people to plan. It would be best if you had your plan. Whatever your goals and objectives are, we want you to reach those goals and objectives. We want your plan to be in place because no matter who you are, healthcare, or tax laws if you do not have your plan in place, someone has a plan for you, and you may not like their plan. Usually, it reverts to the state in which you reside because all states have statutes that apply to healthcare provisions or apply to someone making financial decisions or appointment of guardianships or whatever the case maybe we want to make sure that our clients have their plan in place. We can help clients with emergencies, but we would rather have a plan in place. That is not to say that we cannot help people in emergencies. Having this conversation with the clients can be casual. Suppose you happen to notice someone again has a hole in their planning. Maybe you want to say something. It is not unethical to point out that you may want to consider speaking to someone regarding a healthcare power of attorney, a HIPPA release, or general durable power of attorney. That is different from you promoting yourself as being the healthcare agent under the power of attorney or a financial agent, That is different, but you are simply pointing out that maybe they should talk to someone about getting these things in place because it may be a good idea, and there is nothing wrong with that.
Remember, the healthcare power of attorney is a proxy directive, meaning you are appointing someone to make healthcare decisions if you cannot make your own. That is different from someone on a HIPPA release to obtain information regarding your healthcare. They do not get to make decisions. The healthcare power of attorney can make decisions, someone who is on a HIPAA form can receive information. You may see that if an attorney drafts a document and does not draft a separate HIPAA authorization, they may have HIPAA language in that healthcare power of attorney. That only relates to that acting agent under the healthcare power of attorney. A mom has three kids, and one of the children is appointed the healthcare agent. The medical providers can provide information to that healthcare agent, not to the other two kids. Whereas we draft a separate document That is a HIPPA release, maybe it does have all three kids listed where maybe only child A can make a decision, but all of them can receive information on what is going on with mom or dad. You can only provide information to another individual if there is consent by the patient or if there is a HIPPA release in place where they have authorized in writing, then you are allowed to release information to these named individuals or the agent under a healthcare power of attorney.
Case Study #2- Conflicting Documents
- Tony is a 79-year-old male that was in good health prior to this hospital stay. You meet Tony in the acute care hospital after a prolonged ICU stay related to Covid Pneumonia, he is now in a step-down telemetry unit.
- Tony was intubated, sedated, and proned for 3 weeks. Requiring high flow oxygen therapy post-intubation and has weaned down to 8L humidified O2, however requires a partial non-rebreather for recovery after minimal activity (washing his face, sitting at the edge of the bed, getting to a chair) and BiPap to sleep at night.
- RT is frequently called for additional treatments due to his fluctuating respiratory status.
Tony is a 79-year-old male in good health prior to the hospital stay. You meet Tony in the acute care hospital after a prolonged ICU stay relating to COVID pneumonia. He is now on a stepdown tele-unit. He was intubated, sedated, proned for three weeks, and required a high flow oxygen therapy post-intubation during his hospital stay. He is now on eight liters humidified O2. He requires a partial non-rebreather for recovery after minimal activity like washing his face, sitting at the edge of the night, and using BiPAP to sleep at night. Respiratory therapy is frequently called for additional treatments due to fluctuating respiratory status throughout the day. His arterial blood gases are trending positively towards improved respiratory function. However, his medical condition remains labile. Tony has confusion consistent with ICU-type psychosis. During your respiratory treatments, he has made multiple comments that he does not want to live this way. It is frequently emotional with multiple staff members.
- Tony has 3 children
- Oldest son is the financial agent
- Youngest daughter is the healthcare agent
- Third child has an estranged relationship with Tony
- When family visits, Tony frequently requests family stops his care; however, family refuses to honor this request and Tony remains a full code.
- Physician initiates an ethics committee review of this case to review treatment and course of care.
Psych services have been following Tony, and they have deemed him not competent to make his own healthcare decisions. Tony has three children, his oldest son is a financial agent, his youngest daughter is a healthcare agent, and the third child has an estranged relationship. Tony frequently requests his family to stop his care when the family visits. His family refuses to honor this request, and Tony remains a full code. His physician initiates an Ethics Committee review of the case to review treatment and course of care.
- What is the Realm?
- What is the Individual Process?
- What is the Situation?
Step one, we look at the realm in this situation and apply our RIPS framework, looking at an individual level. We see potentially the patient's wishes not being upheld. We do have the non-competence though of the patient to contend with in this RIPS framework. The organization is involved because of the Ethics Committee's involvement to seek insight and guidance further. In terms of the individual process. We see the moral sensitivity of the patient and the family dynamics and being aware of interpreting that ethical situation. Moral judgment is tricky because the patient is not deemed competent by psych, but the patient expresses wishes frequently to multiple members and is very emotional. The motivation piece of consideration is not something known or unknown. We do have three children, we do have an estranged family, there is reasonable consideration to want to know more, but nothing is glaring in this case in terms of active issues going on. Moral courage is not a piece of the individual process yet that is on the table or in play.
Step two, we look at the situation. We are looking at the end-of-life wishes and the ethical dilemma of a not competent patient. Distress is the main focus of the situation. Is there time for the committee to draw a resolution while this patient potentially is suffering or not having their wishes met in the interim? Reflect on the significance of the legal component and the non-competent patient component.
Step three, looking at deciding the thing to do. Looking at past precedents of care, this is not easy in the COVID population because our care precedence only goes from January to March 2020. Not an area we have a lot of historical data to look at, and all these cases are novel in and of themselves. Also, looking from an institution standpoint, what are further legal implications of Tony's family after a decision is made? Because this is such a novel case, what can happen later on down the line?
Step four, looking at the implementation evaluation and reassessment. We are looking at the patient's preference while deliberating with the committee. This will be the outcome of the Ethics Committee.
- Dueling documents. Which controls? Which is executed latest in time? Does the new document revoke the old document?
- What happens when the Financial agent and Health Care agent under powers of attorney are different people? What if they don’t agree?
- If revoked, notice must be provided to the old agent otherwise, if acting in good faith, decisions of the old agent are valid.
- 46:2B-8.10 Revocation.
- A power of attorney is revoked when the principal has caused all executed originals of the power of attorney to be physically destroyed; or when the principal has signed and caused to be acknowledged in the manner set forth in R.S.46:14-2.1 a written instrument of revocation; or when the principal has delivered to the attorney-in-fact a written revocation. Unless expressly provided, the subsequent execution of another power of attorney does not revoke a power of attorney.
What if the documents conflict? You have to be careful which document you are looking at because you may see general durable power of attorney, but that may be only a financial power of attorney. Some POAs have financial language and healthcare language, but anyone who specializes in this area will have two separate financial and healthcare documents. You could get an attorney who does not specialize in the area and kind of lump everything in together, but for the most part, you will have a financial power of attorney and healthcare power of attorney. If we look at healthcare decisions, we need to look at the healthcare power of attorney. What if there are multiple POAs? Which one was last executed? Did the most recent in-time document revoke the old document? What happens when the financial agent and the healthcare agent are different people? What happens if they disagree?
We have to be careful of what we are looking at, whether we are talking about payment for healthcare or making healthcare decisions. What document are we going to look at there? At any time, these documents can be revoked. The principal can revoke them, assuming that they can do so. If the principal destroys the documents or creates a new document that revokes the old document, if they tell the now acting agent under that document that they have revoked it and they are no longer or should no longer act, any of those types of things can work. The best practice would be to destroy the old document and create a new document in place. Notify the existing agent. Ensure that anyone made aware of the prior power of attorney also has a copy of the new power of attorney. Update their records like banks, insurance companies, medical providers, doctors, depending on whether we are talking financial or healthcare. Sometimes, it can get a little gray as to which one will make decisions or what medical services the client or patient will receive based on the currently controlling document. It may be outside your wheelhouse and what you should be doing, bump it up to your manager and let someone else make that decision if you are unsure what to do.
Case Study #3- HIPAA
- You are treating a patient in the hospital and notice their name is familiar, you recall this individual was active in your church growing up. The patient is in the ICU and very sick. You grew up with the patient’s family and have her son’s number from before, so you call him on your way home from work to check in on him and offer support.
- What is the Realm?
- What is the Individual Process?
- What is the Situation?
Case study three ties all the HIPAA pieces together and reiterates the importance of HIPAA when it is more time-sensitive and or not. To recap, in this case, you are treating a patient in the hospital and notice the name is familiar. You recall the individual was active in your church growing up. The patient is in the ICU and very sick. You grew up with the patient's family and had her son's number from before. You decide to call him on your way home from work to check in on him and offer support. It comes from a genuine desire to do good, but it is illegal.
When looking at the realm, the individual, the patient does not have their privacy protected, and the institution will also be responsible for a HIPAA violation. Applying the RIPS framework, the individual process, moral sensitivity, is being aware that calling to check-in violates privacy. There is wrong moral judgment involving federal laws, financial and civil, and jail time. Motivation, what is causing the person to act out in this way? Are they looking to do a good deed? Is ego involved? The moral courage, if this was a coworker you walking out together, and they are talking to you about the situation, having the courage to stand up and say, "That is not okay to do." The situation, the framework is the temptation piece. It is the temptation to call and check in, reach out, and connect with someone but know because of HIPAA regulations that you cannot.
I certainly would hope that the employee would reflect on it and decide differently from the outcome of this case before an error was made. You would hope they decide to do the right thing and not reach out to that family member. However, under Step four, looking at this patient, this employee did reach out to the family member. There are legal ramifications absolutely, but what was not understood by this employee? Is it a training issue or a genuine lack of judgment? When looking at these situations that come up, looking at the understanding of that individual and training to happen differently.
- “But, I didn’t know”
- It’s no excuse. Whether you’re five or fifty-five, you’ve often responded to an accusation with this sentence
- Unfortunately, in the world of data protection, regulators don’t want to hear that phrase. You must know. When it comes to employee or customer healthcare information, accidents can bankrupt a company
How many of you have heard this, but I did not know. If you have a child, I am sure you have heard that. If the police pulled you over and asked if you knew the speed limit, "I did not know" usually does not work. Whether you are five or 55, many of us have responded to some accusation with this phrase. It will not work, especially in data protection and protected healthcare information. The employee, the employer, or the regulators do not want to hear that.
HIPAA Violations Examples of Social Media
- Unfortunately, there are many HIPAA violation stories that include social media. While social media can be a positive place to share information that can help saves lives, you also need to be very careful about what you share.
- In 2010, a nurse treated a patient with a gunshot wound. The patient was also accused of killing a cop. The nurse took to social media to express her thoughts about the patient on social media. While she left out names, she did post enough details that other social media users could quickly connect her post with news coverage.
- The nurse was fired from her job as a result
We live in a time of social media. While there are many HIPAA violations concerning social media, at the same time, social media can be a positive place. You have to be careful. In 2010, a nurse treated a patient with a gunshot wound accused of killing a cop. The nurse took to social media to express her thoughts about the patient. She left out the names, but she did post enough details that other social media users could quickly connect her post to the news coverage. As a result, the nurse was fired from her job because it was a HIPAA violation. HIPPA includes the patient's healthcare information or information that can lead to that patient's identification. We cannot put information out there that can lead to the identification. Many investigators are out on social media, and they love to figure out precisely what is going on.
- You’d think they’d learn, but in 2017, a med technician wrote a post on Facebook about a car crash victim. Her direct quote was, “Should have worn her seatbelt…”
- While this may seem vague and, yes, seatbelts should be worn, the comment contained enough information that the patient was identified. The med technician was immediately fired for a HIPAA violation
In 2017, a medical technician wrote a post on Facebook about a car crash victim. The quote was, "Should have worn her seatbelt." This certainly seems vague, and we should wear our seatbelts, but the comment contained enough information that the patient was identified. The medical technician was immediately fired for HIPAA violation.
Everyone has seen all of what was going on AstroWorld. After that happened, I saw many medical technicians coming out and responding on social media. Again, you have to be careful with what you are putting out on social media because if there can be a connection, you are violating HIPAA regulations.
- One recent example involves a nurse who created a video in which she interviewed coworkers on the challenges they face working throughout the COVID-19 pandemic in April 2020. One coworker noted that if the hospital had the resources it had requested, a particular patient may not have died, referring to the patient by name
- In another example, an employee from Elite Dental Associates responded to a patient’s review on Yelp, a social media platform for rating and reviewing businesses. The response included sensitive patient information including the patient’s name, treatment plan details, and information about the cost of the treatment and the patient’s insurance. During its investigation of the complaint, the Office of Civil Rights (OCR) found that Elite Dental Associates’ responses to other patient reviews contained similar information. Elite Dental Associates settled the complaint for $10,000
One example involves a nurse who created a video where she interviewed coworkers about the challenges they faced through COVID-19 in April 2020. One coworker noted that a particular patient might not have died if the hospital had the requested resources, referring to that patient by name. We know this is a HIPAA violation, an easy one where you do not say names. Be careful where you are, talking in a cafeteria to other coworkers we may not necessarily know who may be sitting behind us. We certainly have to be careful with our surroundings.
Another egregious example is an employee from Elite Dental Associates who responded to Yelp's patient review. Yelp is a social media platform. The response included information about the patient's name, treatment plan details, the cost of the treatment, and the patient's insurance. An investigation found that Elite Dental Associates' responses to other patient reviews contained similar information. They settled the complaint for $10,000. Even though you may be vague on social media, I would not even go down that road because people can connect the dots. People are good at that. It can be that even though you are trying to be vague, it can be a HIPAA violation. We do not want to take that risk.
Summary
Thank you for joining us today. We certainly hope that we have given you a framework of food for thought in your conversations that come up. We do not expect you to know the answers but have a resource and available folks to help you with that. Our contact information is listed in the handout for you. Please feel free to reach out and connect with us. We would love to continue the conversation.
References
References are in the course handout and can also be downloaded here.
Citation
Bratton, C. & O'Shea, K. (2021). Ethics in crisis. Continued.com - Respiratory Therapy, Article 130. Available at www.continued.com/respiratory-therapy.

