Introduction/Pneumonia Costs
Hello everybody. I am glad to be here. Let's start by talking a bit about the cost of pneumonia.
Dollars
- Mean cost per pneumonia episodes:
- $429.1 for office/outpatient visits
- $1126.9 for ED/urgent care visits
- $10,962.5 for hospitalization
(Tong et al., 2018)
This is some data from 2018 in terms of healthcare dollars. Data two or three years old is considered pretty up-to-date as it takes some time to gather it. The mean costs for pneumonia episodes are hundreds of dollars for outpatient visits, outpatient care, emergency care, and hospitalizations.
- Medicare cost for those with pneumonia during an episode and 1 year after $15,682 higher than age-matched peers without pneumonia; >87 billion dollars cost to Medicare annually (Parks Thomas et al., 2012)
- Annual VHA medical expenditure related to pneumonia = $750 million (>half of which was spent on patients over 65 years of age (McLaughlin et al., 2015)
This is some data from Medicare. They calculated costs not only for the care during the hospitalization for pneumonia but also the accumulating healthcare costs to take care of these folks as they recover. They calculated costs for up to a year. You can see that we are talking about billions of dollars in healthcare costs. We also have some data from the Veterans Health Administration (VHA). They spend millions of dollars in caring for vets with pneumonia.
Mortality
- VHA: Mortality rate = 36% for high-risk patients >65 years of age (McLaughlin et al., 2015)
- 102821 annual deaths in the United States. Mortality at 30 days, 6 months, and 1 year was 13.0%, 23.4%, and 30.6%, respectively
- >1.5 million unique adults being hospitalized annually, 100000 deaths occurring during hospitalization, and approximately 1 of 3 patients hospitalized with CAP dying within 1 year
(Ramirez et al., 2017)
It is not a cost in dollars. We also have to think about cost in terms of lives and mortality rates. This is some data from the VHA. Their mortality numbers are very high, with thousands of annual deaths in the United States and thousands of hospitalizations.
A Serious Problem...But
- Not all pneumonias are aspiration pneumonias
AND…
- Pneumonia isn’t the only possible consequence of aspiration
This is a very serious disease and affects a lot of people. We recognize that pneumonia is a serious problem and has a high cost in dollars and lives lost. However, we need to distinguish between the types of pneumonia as not all are caused by aspiration. And, pneumonia is not the only possible consequence of aspiration. Every aspiration event does not inevitably lead to aspiration pneumonia. As a speech pathologist, I often get consulted when people have pneumonia. It is important to have this distinction.
Some different terms are used in terms used when identifying pneumonia. It is important to understand that not everybody uses these terms in the same way. We have to have conversations with the team (physicians, respiratory therapists, pulmonologists, nursing, et cetera) to build some consensus on defining these terms and using them.
Community-acquired Pneumonia
- Nosocomial
- (Healthcare-associated pneumonia, Hospital associated pneumonia)
- Contracted while in hospital, nursing facility
- Bacterial – often staph
- Recent intubation, ventilation
- Weakness, debility, change in mental status increase the risk
One of those terms is community-acquired pneumonia. These are generally defined as pneumonia following a viral illness that turns into a chest infection. The chest x-ray results are fairly focal, but that is not a necessarily defining characteristic. Certainly, people who are cigarette smokers with underlying lung disease are at higher risk for community-acquired pneumonia. Additionally, individuals who use proton pump inhibitors to manage their reflux are also at higher risk. This is related to the medication decreasing the acidity in the stomach, which has the potential to lead to bacterial overgrowth. These folks are certainly at higher risk than our elderly. There are certain risk characteristics, but really anyone could get community-acquired pneumonia from a viral illness that has progressed.
I want to come back to my earlier point. Not everybody uses the term "community-acquired" in the same way. You can have someone living in the community being treated for a swallowing impairment post-stroke. You may wonder if this is aspiration-related pneumonia. Another person may say it is community-acquired because they were living in the community. Again, we need to know how our team members are using these terms to build consensus.
Nosocomial Pneumonia
Another term we commonly hear is nosocomial pneumonia. You might also hear it referred to as healthcare-acquired pneumonia, healthcare-associated pneumonia, or hospital-associated pneumonia. These are all variations on the same theme. This type of pneumonia is contracted while a patient in the hospital or a skilled nursing facility. Sometimes the definition is expanded to include those folks living in the community but are in health care environments regularly. Examples may be those on renal dialysis and are in the dialysis center three times a week or your head and neck cancer patients who are getting radiation therapy five days a week in the oncology center. These folks are sometimes considered to have nosocomial pneumonia because of their time in the healthcare environment.
If you think about the pathogen, it is typically bacterial rather than viral. And, if an individual goes into the healthcare environment with some weakness or durability or a change in mental status, their susceptibility to nosocomial pneumonia is higher. For example, someone in your hospital who has a urinary tract infection and known dysphagia. They may get pneumonia in the hospital. You may wonder if it is aspiration-related or nosocomial pneumonia. This is why it is important to clarify these terms, at least amongst our own teams.
Ventilator-Associated Risk Factors
- Duration of ventilation
- Tube feedings
- GERD
- GCS<9
Ventilator-associated pneumonia is a subset of nosocomial pneumonia. People who are mechanically ventilated are at higher risk for illness. Risk factors include the duration of ventilation. The longer a person is on the vent, the higher their risk. The risk of pneumonia is higher if they are on tube feeding or have known reflux disease (GERD). Lastly, alertness is another risk with a Glasgow Coma Scale (GCS) score of less than nine.
Infectious Disease Society of America and the American Thoracic Society
- Infectious Diseases Society of America and American Thoracic Society – 2016
- Recommended removal of the concept of healthcare-associated pneumonia
- HAP, VAP caused by different organisms and require different antibiotics
(Kalil et al., 2016)
A few years ago, the Infectious Disease Society of America and the American Thoracic Society recommended removing the blanket term healthcare-associated pneumonia. Their feeling is that what is technically healthcare-associated pneumonia and what is ventilator-associated pneumonia are not the same. They are caused by different organisms that require different types of treatment. As such, lumping them all together under healthcare-acquired or healthcare-associated pneumonia does not make a lot of sense. We still see this terminology being used in facilities, however. Again, you have to know who is using the terms and how they are using them.
"Stroke-associated Pneumonia"
- High incidence of pneumonia in stroke patients…generally thought to be aspiration-related. But…
- Higher incidence of pneumonia in dysphagic stroke patients than in dysphagic patients overall
- Most pneumonia occurs in the acute stroke phase in the presence of a maximum neurological deficit
- So...Is there another mechanism involved?
Another term to be aware of is stroke-associated pneumonia. The first few days after a stroke are a very high risk for pneumonia. It is generally thought to be aspiration-related, as many people post-stroke have dysphagia. However, dysphagia does not really explain the whole picture. There is a higher incidence of pneumonia in dysphagia patients after a stroke than in dysphagia patients overall. Thus, there is something about the stroke that puts these folks at higher risk. Most stroke-associated pneumonia occurs in those first few days. There seems to be something related to the general inflammatory response after a stroke that may be a factor.
- Stroke associated immunodepression
- Infection (particularly fever) leads to neuronal excitotoxicity and electrolyte imbalances which worsen stroke
- Most pneumonia occurs in the setting with the highest degree of disability (within the first 7 days)
- Also…
- Oral flora is altered after stroke – increased colonization overall; changes in bacteria type
(Hannawi et al., 2013; Eltringham et al., 2020
There is also a period of significant immunodepression after a stroke. All of the systems are in an intense inflammatory state. There is also a relation between pneumonia and the degree of disability as most stroke-associated pneumonia occurs in those with the most disability and those first few days. Interestingly, we also know that some important oral bacteria/flora changes occur right after a stroke. This is most likely related to the immunodepression and generalized inflammatory response. There is more colonization of bad bacteria, if you will that could be contributing. It is complicated with several things going on there.
COVID Pneumonia
- More likely to be bilateral
- Significant ground-glass opacities on CT
- “Silent hypoxia”
We are now seeing COVID pneumonia. This type is more likely to be bilateral. It is related to the COVID infection, and on imaging, we see significant ground-glass opacities. The important characteristic of COVID pneumonia is what has been termed silent hypoxia. These are folks who have very low oxygen saturation but are not necessarily perceiving significant dyspnea. People with COVID pneumonia are not always the best judge of their saturation status.
Aspiration Pneumonia
- Aspiration Pneumonia
- Can be Nosocomial or Community Acquired
- No consensus re: diagnostic criteria
- No “gold standard” for assessment and diagnosis
- Aspiration of colonized oropharyngeal material (food, gastric contents, secretions)
- Pulmonary inflammation in response to bacteria
- CXR: Opacities in dependent portions of the lung (LL, posterior UL)
- Dysphagia, gastric dysmotility are risk factors
- And…
The next is aspiration pneumonia, a common one with SLPs. Aspiration pneumonia can be either nosocomial or community-acquired. There is no consensus or gold standard for assessment. And it is challenging to determine specifically what causes pneumonia. When we think about aspiration pneumonia, this is caused by aspiration of secretions, food, or gastric contents.
Reflux is an important risk factor for aspiration pneumonia. On a chest x-ray, you are likely to see opacities in the dependent portions of the lungs. This means that gravity is taking that aspirated material as low as it will go. As an example, lower lobe pneumonia is most likely a result of aspiration. Every lower lobe pneumonia is not aspiration-related, but that certainly is part of the process that physicians go through as they are ruling out the cause.
You also have to think about how the patient is positioned. Suppose this is someone who is bed-bound and spends a lot of time and recline. Where is gravity going to take that aspirated material? It is more likely to be in the posterior upper lobe. In contrast, people who have dysphagia are at higher risk for aspiration pneumonia, as are individuals with gastric motility or reflux problem.
- Associated with Acid-Suppressive Medication
- PPI use results in higher bacterial load in gastric contents
- Aspiration of gastric contents, then, results in aspiration of large amounts of bacteria
There is a relationship between acid-suppressive medications like proton pump inhibitors (PPI) and aspiration pneumonia. Individuals taking proton pump inhibitors usually have some known gastric dysmotility or a known reflux problem. These medications make the reflux less acidic, but they do not stop the backflow of the reflux site. They just make it less acidic, so there is less damage to the esophagus. This backflow of stomach contents, although less acidic, has bacterial overgrowth in it and can be aspirated. With this, you are likely to get sick.
Pneumonitis
- Chemical Pneumonitis/Aspiration Pneumonitis
- Lung inflammation resulting from aspiration of acidic and/or particulate gastric contents (20-25 ml of material of pH>2.5)
- LOC (including post-surgical, seizure, CVA
- Respiratory distress within minutes/hours
- Subsequent bacterial infection in some
There is a distinction between pneumonia and pneumonitis. You may see the term chemical pneumonitis or aspiration pneumonitis. In fact, chemical pneumonitis seems to be replacing aspiration pneumonitis. Pneumonitis is an inflammatory process as the result of aspiration of large amounts of acidic stomach contents. The person is usually not awake or very alert. This may occur with the college student who drinks until he passes out, vomits, and aspirates. Or, this could be the patient that has a seizure, loses consciousness, and aspirates vomit. This could occur if a person does not fast due to emergency surgery and vomits during the procedure. Pneumonia can take a while to percolate, but these folks with pneumonitis are in trouble right away. They are short of breath and in respiratory distress minutes to hours after the aspiration event. In some people, this progresses to a more diffuse bacterial infection, but initially, it is more of an inflammatory process.
Is It All About The Coding?
- Much variability in how aspiration pneumonia is diagnosed and coded:
- Physicians often have difficulty diagnosing pneumonia etiology
- Aspiration pneumonia and pneumonitis can be difficult to differentiate clinically
- Regional differences in practice observed
- And…
- Aspiration pneumonia typically associated with higher payment rates
(Lindenauer et al., 2018)
We do not really have a good handle on pneumonia types because of all of the variability of how these terms are used and coded. It is not an easy thing to determine exactly what is causing pneumonia, and this contributes to some of the variability. There are some regional differences as well as differences in reimbursement. Community-acquired pneumonia and aspiration pneumonia have different reimbursement levels, as one example, and aspiration pneumonia is typically billed higher. As such, there may be a tendency to err on that side of caution/profit and get paid the higher rate. As you can see, many external factors can confuse diagnosing and billing for pneumonia.
GERD and Aspiration
- Pulmonary Consequences of Aspiration of Gastric contents:
- Asthma exacerbations
- COPD exacerbations
- Chronic cough
- Bronchiolitis
- Respiratory difficulties
- And…
- Pneumonia
I want to come back to this idea of reflux disease and aspiration. The consequences of aspirating stomach contents are significant. This can result in pneumonia, as we have been discussing. We also know now that even microaspiration of acidic stomach contents can exacerbate asthma, making it harder to control. It can also result in exacerbations of COPD and hospitalizations related to COPD exacerbations. It can cause chronic cough, respiratory, and bronchiolitis. The point is that many physicians and healthcare teams tend to focus on swallowing and the aspiration of food and liquid. I am not saying that is not important. Still, we need to broaden our perspective a bit and think not just about prandial aspiration but also about the aspiration of stomach contents. Getting reflux under control is going to be an important treatment consideration.
Something Else To Consider
- 25 patients with occult aspiration as diagnosed via lung biopsy
- 96% had GERD
- 40% had esophageal dysfunction
- 40% had oropharyngeal/laryngeal dysfunction
- 32% had HH
- 32% Obstructive sleep apnea
- Radiological presentation = multilobar/centrilobular nodularity, tree in bud, airway thickening, and fibrosis (less commonly)
(Cardasis et al., 2014)
This study is from a few years ago. The subjects had undergone lung biopsies and were found to have aspirated materials, both food and liquid. They did a retroactive study to see which individuals were not known to be aspirating. They found that 96% of them had reflux disease, 40% had some esophageal dysfunction, 32% had a hiatal hernia, and 40% had oropharyngeal dysfunction. Again, I am not saying that we do not have to worry about dysphagia. I am only saying it is not the only thing we have to worry about. Obviously, many of these folks had more than one thing going on, which was probably a contributing factor to their difficulties as well.
Aspiration-Clearance Mechanisms
- Cough
- Mucociliary escalator
- Cellular defenses
What happens in your lungs when you aspirate, and what are the pulmonary clearance mechanisms. Cough is the primary protective mechanism against aspiration. We use a cough in two ways. We use cough to keep material out of our airway and to get material out of our airway. If we aspirate and the material is in the trachea or even in the first few bifurcations on the bronchi, we have the potential to use a cough to clear the airway. And, you are going to cough regardless of what it is you are aspirating. It does not matter to your airway if the material is coming down from your mouth or up from your stomach. The healthy airway is going to respond.
Once we have aspirated and the material is deeper in the lungs beyond where the cough response can respond, the mucociliary escalator and cellular defenses. These two systems work simultaneously. The cilia are coated with mucus and have the potential to catch and trap the aspirated material. Then, the wave-like motion of the cilia and the lung fluid brushes that mucus impregnated aspirate up to the point where you can then cough it out. At the same time, we also have cellular defenses working. These cellular defenses are mediated by your immune system, which sends white blood cells. There are several different types and subtypes of white blood cells, but some of them can complete phagocytosis on the aspirated material and even bacteria.
If these three systems fail and the aspirated material is not cleared, then you get sick. A patient with aspiration pneumonia has failed pulmonary clearance mechanisms.
Aspiration and the Airway
- Laryngeal Penetration:
- Frequent occurrence in normals
- Increases in frequency for larger liquid boluses
- Frequency increases with age (>50 yrs)
- (Daggett et al., 2006)
- AND…
- As many as half of the healthy adults aspirate small amounts of their secretions...usually in our sleep (between 0.1 and 2 ml) (Gleeson et al., 1997)
I want to make a distinction between laryngeal penetration and actual aspiration. We use the term penetration to refer to that material that gets into the laryngeal vestibule but does not get past the vocal folds or enter the trachea proper. We know that laryngeal penetration material that enters the laryngeal vestibule and eventually gets cleared is a frequent occurrence in normal swallowers. It happens a lot, especially with larger bites and sips and straw drinking. This is also more common in older people. We also know that aspiration is a fairly normal occurrence. I am not suggesting that everybody is constantly aspirating but everybody aspirates once in a while. I am sure you have experienced this while talking or laughing when eating and not paying attention to what you were doing. Most of us have also aspirated some of our saliva in our sleep. However, we are not all walking around with aspiration pneumonia because of those pulmonary clearance mechanisms that we just discussed.
How Much Aspiration Is Too Much?
If everybody aspirates some and we have the potential to clear aspirated material, this begs the question, "How much aspiration is okay, and how much aspiration is just too much?"
- What was aspirated?
- Acidity
- Fat molecules vs. Water molecules
- Weight
- Bacteria
As we have said, aspiration of acidic stomach contents is very dangerous in the lungs and very hard to clear. Thus, getting the reflux under control is going to be an important strategy to reducing pneumonia risk. What about the aspiration of food and liquid? Everybody is always concerned about this, and certainly, as a speech-language pathologist, I spent a lot of time thinking about it. It matters what you aspirated. You can think about this as a continuum of safety. There are fairly safe things at one end of the continuum and others that are more dangerous at the higher end of the continuum. One thing that is fairly benign in your lungs is water. Water is pH neutral, and some of it seems to be absorbed by the lung fluid. There also are molecular channels called aquaporins that have been identified as having a role in channeling water out of the lungs and back into the bloodstream. I am not saying you can pour water into the lungs, but the amount you are likely to aspirate while you were having a drink will be fairly well tolerated.
In terms of risk continuum, up from that would be those foods and liquids that have water-based molecules. These would be things like fruits and most vegetables. They are not as safe as water but safer than those foods and liquids at the higher end of the continuum.
Fatty-based and protein-based molecules are higher on the continuum as they are not very well cleared. This is about phagocytosis and those white blood cells scavenging through the lungs. If the aspirated material is water-based, the absorption occurs much more efficiently. We also have to think about the weight of the aspirated material. This is about mucociliary clearance and the cilia brushing that mucus impregnated aspirate up and out. This process is going to be less efficient with heavier particles. As we know now, people who aspirate food are more likely to get sick than people who aspirate liquid. Additionally, we know that people who aspirate thick liquids, a common intervention for people with dysphagia, are more likely to get sick than people who aspirate thin liquids. As we think about putting a thick liquid intervention into place, we have to make sure that it works. If you put a thick liquid intervention into place and the person is not aspirating that, then we do not have to worry about pulmonary clearance. If this person is still aspirating and the thickened liquid is not doing its job, we will probably do more harm than good. Thick liquids in the lungs are now going to be much harder to clear, and we are putting this individual at higher risk. The moral of the story is that if we put a thick liquid intervention into place, we have to be sure that it is working.
Finally, we have to think about not only the aspiration of something like applesauce but, more importantly, what bacteria might that apple sauce have carried down with it as it traveled through the oral cavity. A moment ago, I said water was pretty benign in the lungs. The caveat is that the water has to be from a clean mouth. If that water had to travel through an oral cavity that has not had a toothbrush in it in weeks, then that water is toxic with many bacteria. Therefore, whatever is aspirated is going to be an important risk factor to consider.
Two-tier Assessment Process
- Two-tier Assessment Process:
- What is the likelihood that this patient is aspirating?
- What is the likelihood that this patient will develop aspiration pneumonia?
What I am advocating for is a two-tier assessment process. First, is the person aspirating? If the answer to the first question is yes or probably, what is their potential for pulmonary clearance? Is the aspiration more or less likely to result in illness? Notice that I am talking about the likelihood. No one can look at a patient or a swallow study and say, "You are aspirating, and that aspiration is definitely going to make you sick." Nor can someone look at that same swallow study or that same patient and say, "You are aspirating, but do not worry about it. That aspiration is not going to make you sick." Nobody can talk definitively at this point. However, we can think about the likelihood. In other words, what is this individual's potential for pulmonary clearance? If they have good potential for pulmonary clearance, then the likelihood that that aspiration will result in illness will be lower.
Aspiration Framework
Figure 1 shows the framework that we want to think about.
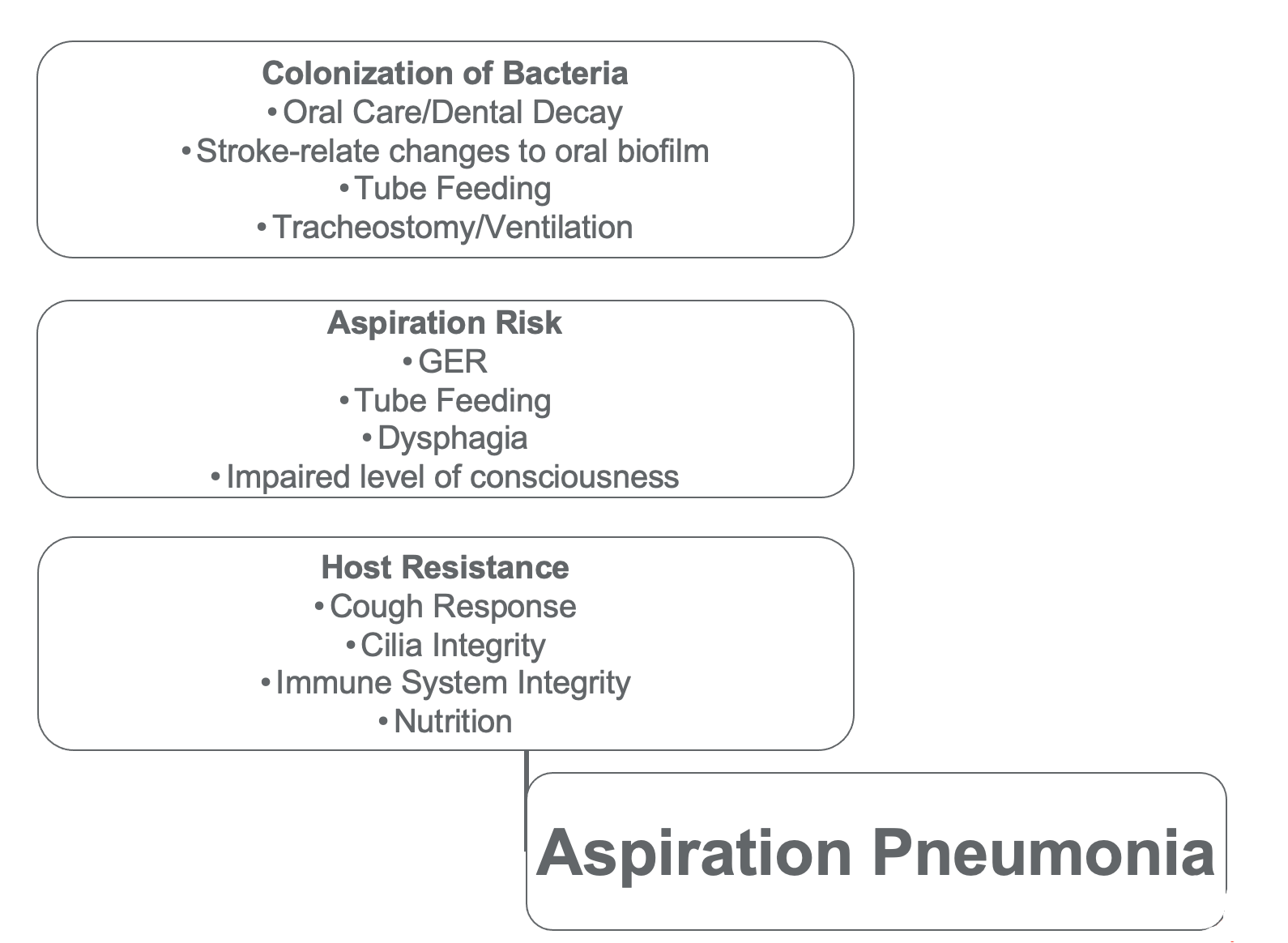
Figure 1. Aspiration framework.
Colonization of Bacteria
For aspiration pneumonia to occur, three things have to happen. There have to be some bacterial stores that are aspirated and not cleared. We can think about identifying patients who are at risk by looking at this framework. Where is the bacterial source? Do they have a lot of dental problems and do not take care of their teeth? Are they dependent on oral care, and nobody is taking care of their mouth? Is this someone who just had a stroke and may have some of those stroke-related changes to their oral flora? Is this someone who has a feeding tube, a trache, or vent tubing? We know bacteria love dark, warm, wet places. While we do our best to keep that clean, bacteria can collect there and migrate. Bacteria can make a short trip from the vent tubing or the trache tube to the oral cavity/pharynx, where then it becomes part of whatever is aspirated. In summary, we know that the presence of tubes, a new stroke, and people who do not have good oral/dental care will be at higher risk here due to bacterial.
Aspiration Risk
Step two is the bacteria has to get into the lungs. Folks with pharyngeal dysphagia or known to be aspirating while they eat and drink are at risk here. Folks with known reflux disease and those being tube fed and refluxing, as a result, are also at risk. We also have to look at those who are not awake and alert.
Host Resistance
Those two things alone will not result in illness. Those without pulmonary clearance are at higher risk. Who cannot do that? The first one to look at is cough. Many people do not have a good clearing cough. They may have impaired laryngeal sensation and are what we call silent aspirators. They aspirate without any cough response at all. Others have a weak cough response due to respiratory/trunk muscle weakness. The second pulmonary clearance mechanism was mucociliary clearance. Folks with poor ciliate integrity are not going to be able to do that very well. These are the individuals that are cigarette smokers, have COPD or emphysema, or are dehydrated. Dehydration does not damage the cilia per se, but it certainly decreases the motility. Remember, the cilia move in the lung fluid. If a person is dehydrated and their lung fluid is diminished, their cilia do not move very well. When we rehydrate, the cilia will begin to move again. However, during that period of dehydration, there will not be good mucociliary clearance. The last pulmonary clearance mechanism is phagocytosis, or the immune system response. Folks that are immunocompromised or some other infection going on are not going to have a good response. People who are malnourished, generally debilitated, or have a high degree of disability will also demonstrate a decreased immune response.
Aspiration Framework-Elderly
- Dependence for oral care; Reduced access to dental care
- Higher risk of conditions causing dysphagia
- Age-related changes to the respiratory system and immune system
Let's now superimpose our aging population on this framework (Figure 1). If you think about all of those risk factors, we know that the elderly are more likely to be dependent on oral care and therefore do not get good oral care. Often, as folks transition away from private insurance to Medicare, they lose their dental insurance. They might have less access to dental care as a result. They are at higher risk for conditions that might cause oral pharyngeal dysphagia, like a stroke or neuromuscular disease (Parkinson's disease, dementia, etc.). We also know that as people age, their respiratory system and immune systems become a little less efficient. If you superimpose what happens in aging onto our framework, you can see how the elderly have a particularly high risk of developing pneumonia.
Aspiration Tolerance
- Consider overall medical condition, medical stability
- Consider nutritional status (immune system function)
- Consider hydration status (cilia movement)
- Consider pulmonary status
- Consider oral hygiene
The first question to ask is, why are they aspirating? We also have to put that aspiration in the context of the potential for pulmonary clearance. We need to look at an individual's overall medical condition and comorbidities. We have to look at their hydration and nutritional status. We also need to look at lung function and oral hygiene. Lastly, we have to put the aspiration risk in the context of the aspiration pneumonia risk and the potential for pulmonary clearance. This is something that we do as a team, and everybody has to contribute to this part of the assessment process.
What Can We Do?
- Medications
- Early ID/Screening for dysphagia
- Head of bed elevation
- Oral hygiene
- Nutrition/Hydration
- Free Water
What are some of the things that we can do in terms of prevention and management to keep folks from getting sick in the first place? This is what we are going to talk about in the second half of our talk today.
Interventions: Medications
Can Medications prevent aspiration pneumonia?
- No...
- Prophylactic antibiotics were not effective in preventing aspiration pneumonia (Kalra et al., 2015)
- Maybe…
- Prokinetic medications may prevent aspiration pneumonia in tube-fed patients (Liu et al., 2017)
- ACE inhibitors are inconsistently effective in increasing cough response and reduce aspiration pneumonia risk
- Effect most likely in patients of Asian descent and patients with previous stroke (Caldeira et al., 2012)
Researchers found that mixed prophylactic antibiotics were not very effective in preventing aspiration pneumonia. There is a little bit of evidentiary support for prokinetic medications. These speed up stomach emptying and may decrease aspiration pneumonia in individuals who are being tube-fed. ACE inhibitors are used to manage heart disease and hypertension. They are commonly prescribed in elderly clients. People who take these medications often complain that they have an irritating cough as a result. ACE inhibitors seem to increase cough sensitivity and response. There is some mixed evidence to suggest that these ACE inhibitors, by increasing the cough response, may decrease pneumonia risk. There is also some mixed evidence that ethnicity may play a role in responding to these medications. Nobody is at the point where they are prescribing ACE inhibitors, but it is an interesting consideration.
Substance P
- Peptide that transmits signals from sensory nerves to CNS
- Important for pain transmission, emotional responses, cough, and swallow
- Reduced in patients with dysphagia (Kishida, et al., 2013)
- Low Substance P in stroke patients correlated with low frequency of spontaneous swallowing (Niimi, et al., 2018)
- Beta-blockers may increase Substance P levels and protect against dysphagia (Miarons, et al., 2018)
ACE inhibitors seem to increase substance P, which is a peptide that acts as a neurotransmitter. It is essential for transmitting sensory information around pain, emotional responses, and cough and swallow. We know that in patients who have dysphagia, substance P levels are often reduced. This has been studied in stroke patients in particular. Increasing substance P levels increases the transmission of sensory information and cough response. This is an exciting area of research that I think we will hear more about.
Intervention: Swallow Screening
- Not a replacement for the Clinical Swallow Evaluation
- ID’s patients in need of full assessment
- Should probably include:
- Assessment of level of alertness, ability to participate
- Observations of swallows
- Observation for change in vocal quality, cough
The next tool in our toolbox is a swallow screening. As a speech pathologist, I feel like I have to say this is not a replacement for a full swallow evaluation, but it does help identify patients at risk so that they can be evaluated. There are all kinds of screening tools out there that are validated on different populations. In general, a good swallow screening should include assessing the level of alertness, an observation of swallowing (usually with water), and some observation for clinical signs of aspiration. These are things like cough or wet vocal quality.
Review of Water Swallow Tests
- Compared water screens with smaller (single sips) and larger boluses (3 oz)
- Larger boluses: Good sensitivity in determination of aspiration risk
(Brodsky et al., 2016)
Dr. Brodsky reviewed all of the water swallow screening tools out there and the different protocols a few years ago. He found that when they looked at the water screens that involved individuals taking smaller sips compared to those taking larger boluses, the three-ounce water tests (larger boluses) had good sensitivity in determining aspiration risk. The Water Swallow Test is probably the most commonly used in facilities.
- Useful in the identification of patients needing full clinical assessment
- Reduce pneumonia rates in facilities that use them
(Hinchey et al., 2005; Schrock et al., 2018)
Screenings seem to have some evidence to support their use in identifying folks who need a full assessment. We know that in facilities where a swallow screening process is in place, pneumonia rates go down. If we can identify these folks at risk for aspiration early and put management strategies in place, we can decrease pneumonia rates.
Intervention: Head Of The Bed Elevation
- Conventional wisdom – elevate the HOB to improve airway protection during eating, tube feeding to reduce aspiration risk
- Also, to reduce the risk of aspiration of nocturnal refluxate
- But does it really work?
The next one to think about is head of the bed elevation. If we keep the head of the bed elevated, it will help improve airway protection when folks are eating or being fed through a tube. It may also help to decrease the reflux that occurs during sleep. Here is some of the evidence.
- Yes…
- Intubated/ventilated patients - pneumonia rates lower in the semi-recumbent group as compared to supine (Drakulovic et al., 1999)
- HOB elevation decreased pneumonia rates in hospitalized patients (Patty et al., 2021)
- Yes but…
- Elevation of HOB reduces the risk of aspiration, but the required degree of elevation unclear: 30 v 45? (Blot et al., 2014)
- No, but…
- A review of the literature found no significant benefit but no harm as long as it does not interfere with other medical interventions (Niel-Weise et al., 2011)
The evidence is mixed. Does elevating the head or keeping the head of the bed elevated prevent pneumonia? There is some evidence to suggest that it does. You can see a couple of studies (one very recent study) found that keeping the head of the bed elevated does reduce pneumonia rates. The 2014 study demonstrated the elevating the head of the bed reduced the risk of aspiration, but there was no clear guidance in terms of how high the head of the bed needed to be. A review was done a few years ago that found that it does not really make a difference after all. Logically, it seems like it should help due to gravity.
- Yes…
- 20 cm blocks under bed reduced acid exposure, increased acid clearance time, improved sleep (Khan et al., 2012)
- 6-inch elevation reduced or eliminated reflux episodes (Scott et al., 2015)
- Compared 30 and 45-degree elevation in G-tube fed mechanically vented ICU patients – higher elevation reduced reflux without pressure ulcer development (Schallom et al., 2015)
- A systematic review revealed a decrease in GERD symptoms and improvement as measured by pH studies (Albarqouni et al., 2021)
Certainly, it makes sense in terms of reflux management. If we think about not just the aspiration of food and liquid but also the aspiration of anything, including reflux, then there is a compelling argument to be made for keeping the head of the bed elevated. You can see there are some studies, including some systematic reviews, that say that keeping the head of the bed elevated keeps the reflux down, and therefore, it keeps the risk of aspiration of the reflux down.
- Improving Compliance:
- RN “Champion” (DeLuca et al., 2017)
- Multidisciplinary approach (Khan et al., 2016)
- Bed without HOBE measuring device (Llaurado-Serra et al., 2015)
- Beds with side-of-bed rather than an under-bed measuring device (Fitch et al., 2016)
If we broaden our scope and want to keep our folks from aspirating, bed elevation becomes important. The problem is that it is tough to do. Facilities that do keep the head of the bed elevated successfully make it a multidisciplinary approach. In other words, it needs to be a priority for everybody, even those doing patient transportation. There is a big risk factor for head of bed elevation management during transitions from room to room or from their room to radiology or another procedure. This is when the risk is highest in terms of compliance. And, some beds have elevation measuring devices that can complicate things. You can see the research is mixed in terms of how effective those are.
Intervention: Oral Hygiene/Aspiration of Oral Bacteria
Healthy Adults
- Healthy adults aspirate saliva in their sleep commonly…typically does not lead to disease
- But with hospitalization and/or illness…
- Changes in oral microbes (more virulent organisms)
- Immune compromise
- Fatigue
- Disruptions in regular oral care routine
Another important consideration in keeping the aspiration risk down is the management of oral bacteria. Everybody aspirates, but most are not getting sick due to good oral care and health overall. Additionally, most people have healthy immune systems. Folks hospitalized or have some sort of illness are immunocompromised or tend to have more bad bacteria in their oral cavity. They are tired and cannot always get the oral care done as well. They may not be brushing their teeth regularly or getting to the dentist. If they are immunocompromised this can lead to an overgrowth of bad bacteria as well. Good oral care in individuals who are at risk can help to keep the pneumonia rates down.
Evidence in Hospitals
- Nurse-driven oral care program for all hospitalized patients (including ventilator-dependent patients)
- Resulted in decreased LOS, decreased cost of care, and decreased mortality
(Warren et al., 2019)
This study was a nurse-driven oral care program for hospitalized patients that included a subset of ventilator-dependent patients. This not only decreased pneumonia rates but decreased the lengths of stay, decreased the costs of care, and decreased mortality rates. This is one way to get your administrators on board.
Evidence in Stroke Patients
- Intensified oral hygiene program lowered the risk of stroke-associated pneumonia
(Yuan et al., 2020)
Here is some research that looked at an intensive oral hygiene program that lowered the risk of stroke-associated pneumonia.
Evidence in ICUs
- Chlorhexidine rinse or gel likely reduces VAP incidence
- Toothbrushing may reduce VAP incidence and may reduce the length of ICU stay
- No evidence for impact on mortality
- (Zhao et al., 2020)
- Toothbrushing reduces VAP as compared to swab/gauze
- (De Camargo et al., 2019)
Here is some of the research on critical care patients. Chlorhexidine is a very intense antibacterial rinse that comes in a gel form. If you have ever had a crown or a root canal, it is a nasty tasting rinse that is very good at killing bacteria. This medication does seem to reduce ventilator-associated pneumonia, at least in this study. Tooth brushing is also important, as you can see above. In some cases, it is really about friction. The friction of the toothbrushing helps to get that bacteria get that biofilm off of the teeth and gums. Foam/dental swabs are commonly used in critical care units. However, they are not as effective because you cannot get as much friction as a toothbrush. The toothpaste is not as critical, so if you are worried that someone might aspirate the toothpaste, do not use it. A wet toothbrush will be just as effective.
- Chlorhexidine may increase mortality- perhaps due to cytotoxicity
(Klompas, 2019; Vieira et al., 2020)
We have to be careful, however, about chlorhexidine. It does seem to have some toxicity associated with it. While it is a powerful antibacterial, we want to use this very cautiously and only when prescribed by physicians. We would want to reserve it for those cases where oral hygiene is really terrible. A wet toothbrush is probably going to be our best tool.
Evidence in Skilled Nursing Facilities
- “Mouthcare without a Battle”
- Includes staff education, toothbrushing, denture care, designation of “oral care aide”
- Training re: care-resistance behaviors
- Reduction in pneumonia rates in the first year of implementation; less so over year two…
- Sustainability of the program?
Here is some of the research in skilled nursing facilities. If you work in skilled nursing facilities, you know that oral hygiene can be a challenge for folks who have cognitive impairment. They have what is termed care-resistant behaviors. As dementia progresses, we see more and more deterioration in terms of critical function. Many of the brainstem functions are preserved, including the functioning of the amygdala. The amygdala is part of the brain stem and has a significant role in alerting a person to danger. For those who have intact, critical functions, we can mediate the danger signals from the amygdala. Your amygdala may warn you when someone is approaching your mouth with tools like a dental hygienist, but we can override that. Folks with dementia start to lose that cortical function. Their amygdala is screaming, "Danger!" but they have no cortex function to override that a clinician is helping them with their hygiene. This is why you see so many fear-based care resistant behaviors as dementia progresses.
It is tough to get oral care done in skilled nursing facilities. This is some research around a program called Mouthcare without a Battle. It is a multidisciplinary, multi-dimensional program that involves staff education and regular toothbrushing guidelines for denture care. It also designates individuals in the facility who are the oral care aids. They help facilitate staff with this program and receive specific training around managing those care-resistant behaviors by using specific responses to those fear behaviors. By doing this, there has been a demonstrated reduction in pneumonia rates over the first year of implementation of the program. However, the outcomes started to deteriorate as time went on. Factors causing this decline were that it is hard to implement and sustain a high level of attention. There are competing priorities, staff turnover, and hard to keep that education going. Keeping these kinds of programs in place seemed to be the challenge. We can do it for a period of time, but we cannot sustain it all the time.
- Cost
- Staff time
- Toothbrushes, toothpaste
- Adaptive equipment
- Rinses, etc.
One of the things we get push back about for oral care programming is the cost. When you start talking about staff time and supplies (toothbrushes, toothpaste, suction oral care, and adaptive equipment), the costs start to add up.
- Cost of NOT doing good oral care
- Remember?
- Pneumonia = >87 billion dollars cost to Medicare annually
However, remember what we talked about at the start of this presentation. We are spending billions of healthcare dollars to manage people with pneumonia. If we can use a simple tool like a toothbrush or suction oral care to keep this cost down, it seems like it would be a cost-effective intervention.
Intervention: Nutrition/Hydration
Undernutrition
- Immune compromise
- Increased pneumonia risk
Nutrition, nutritional compromise specifically, and immunocompromise are related. Your immune system is fueled by good nutrition. We have also established that when someone is immunocompromised, they have decreased pulmonary clearance and higher pneumonia risk. There is clearly a link between nutritional status, the immune system, and pneumonia. Can we improve nutrition to therefore improve someone's immune system functioning? This leads to texture modification, modified diets, and some other tools for managing individuals with dysphagia.
Texture Modification
- Can result in decreased intake and nutritional compromise
- Assistance to the family for caloric/protein density
- Consider personal preferences
Perhaps, we prescribe thickened liquids to keep the person's swallow safer. But in fact, these modifications may actually increase nutrition and hydration risk. For one, people do not like them. Puree diets are not very appetizing, interesting, visually pleasing, or taste good. When you have to bring texture down to a pureed level, you have to add fluid. This causes a dilution of caloric and protein density as well as a dilution of flavor intensity. Pureed diets are often lower in calories, protein, and taste. In many facilities, they have particular recipes to add calories and protein, but the taste does not always get addressed. And certainly, if you have families trying to manage a pureed diet at home, it can be challenging to keep calories/protein up while at the same time trying to keep the texture down. Thus, the invention that we are putting into place to keep the person's swallow safer may actually cause them to eat less and become nutritionally compromised. This puts them at higher risk for pneumonia that we are trying to prevent. We have to think very carefully about the interventions that we need to make.
Non-oral Feeding
- Not without complications…
- High mortality in neurological, dementia, and cancer populations
- Increased medical intervention, support
- Potential for complications (reflux, pain, bleeding, infection, to name a few)
- Caregiver burden
- Effect on quality of life?
What about non-oral feeding/tube feeding? This is not without its own set of complications. Certainly, you are bypassing the upper part of the digestive system. There is a sense that this must be safer from a swallow perspective. However, there are several complications associated with non-oral feeding. There is higher mortality in certain populations. It also requires a higher degree of medical intervention and caregiver support. There is also increased reflux, as we have talked about. There can also infection and discomfort at the site, increasing caregiver burden and decreasing the individual's quality of life.
If you stop to think for a moment about some of the social activities you enjoy, I would guess that most, if not all of them, involve some sort of food or drink. Food keeps us alive, but it is also a social tool. Celebrating the holidays and getting together with friends and family all involve eating or drinking. When that is not available, social relationships can suffer not only for the individual but also for the family members/caregivers.
Tube Feeding and Dementia
- No evidence that tube feeding
- Improves nutrition
- Increases life expectancy
- Reduces risk of pneumonia
- Improves functional status
(Cochrane Review, 2009)
There has been quite a bit of research around non-oral feeding in patients with dementia. There is no evidence that tube feeding improves nutrition, improves life expectancy, decreases pneumonia risk, or has any positive impact on the functional status of patients with middle to end-stage dementia. You provide nutrition through a tube, but the body is breaking it down and simply cannot metabolize it. There is no good clinical reason to think about non-oral feeding for patients with middle to end-stage dementia.
- Tube Feeding- Guidelines for Practice
- Consider other options:
- Hand-feeding when the patient is awake, alert
- Pleasure feeds
- Oral care to improve comfort
- Pain control
- Skincare
- Consider other options:
We have to think about some other options for nutrition. There is a movement toward "eating with acknowledged risk." This translates to careful assistance for oral feeding. When the patient can participate, you want to encourage them to eat for pleasure, rather than necessarily eating for nutrition. These programs generally involve oral care as again. We want to keep their oral cavity as free from bacteria as possible. These programs also usually involve some aspect of pain control to keep people comfortable and, therefore, better participate. It is also important to monitor their skin as we know that they are more at risk when their medical status is deteriorating due to nutritional compromise at the end stages of diseases.
Aquaporins
- Molecular channels that transport water via osmosis
- Found in various areas of the body – kidney, gi organs, lung
- In infant lung, important in the facilitation of transition from fluid secretion to fluid absorption; Aquaporins increase dramatically near term
- Aquaporin expression reduced in inflammatory lung disease, including COPD
- Responsible for:
- Airway hydration
- Airway defenses
- Reabsorption of excess alveolar fluid
- Do not seem to have a role in the management of infection or edema
(Day et al., 2014; Verkman et al., 2000)
I want to come back and talk a little bit about water. I mentioned earlier in the talk that there are molecular channels called aquaporins. They are found not just in the lungs but also in various other parts of the body, including kidneys and the gastrointestinal system. They seem to have a really critical role in infancy. They help the infant transition from fluid secretion, which happens in utero, to fluid absorption once the baby is born. The production of aquaporins in the fetal lung increases dramatically as the baby nears term. Then, we continue to see aquaporins throughout the lifespan, although not to the same degree. For example, sometimes inflammatory lung diseases, including COPD, have the potential to decrease aquaporin expression. Why do we care about them? Aquaporin channels seem to have an important role in airway hydration, reabsorption of the excess alveolar fluid, and perhaps the management of water aspiration, as we were talking about earlier.
Intervention: Water Protocols
Aspiration Management Diets- Frazier Water Protocol
- Rehab patients who are NPO or on a dysphagic diet
- Water is unrestricted prior to meals and 30 minutes after a meal
- Medications are given in puree, or with thickened liquid, not with water
- Manner of presentation of free water may be restricted – e.g., by teaspoon only
- “Aggressive oral care”
- Outcomes = increased pt. satisfaction, increased hydration, no increase in pneumonia rate
This information has led to the development of what are called water protocols. Above is the Frazier water protocol that was developed at Frazier Rehabilitation Hospital. This protocol is for individuals who have known dysphagia or have been evaluated for dysphagia. These individuals are encouraged to drink unthickened water. If they recommend thickened liquids, they will get those liquids with their meals and medications, but outside of that, they would be encouraged to drink unthickened water. If they get their nutrition via an NG-tube or G-tube, they would be encouraged to drink unthickened water by mouth. Some people refer to these as free water protocols. People may think that everybody is guzzling water from gallon jugs, but that is not the case. The evaluation of the swallow function results in some recommendations for the water. It might be that this person can drink water independently, while another person might need supervision or need a cup or a straw. Some individuals may need to keep the volume down by using only a teaspoon or ice chips.
We can manage how the individual gets the water, but everybody gets water. We know the risk of aspiration is there. With dysphagia, the person will likely aspirate some of that water, and that is okay. However, we do not want that to happen at lunch where the person asks for the water, and it washes down some of that pork chop. That is not okay. We do not want the person to drink regular water when swallowing pills. However, outside of meal times and medication, water is encouraged. The key to the success of this program is oral care. A fairly aggressive oral care program goes hand in hand with these water protocols. Again, water from a clean mouth is going to be very well-tolerated and managed by the lungs.
Water Protocols – What’s the Evidence?
- Increased fluid intake (Garon et al., 1997; Karagiannis et al., 2011; Carlaw et al., 2012; Karagiannis et al., 2014)
- Improved QOL (Karagiannis et al., 2011; Carlaw et al., 2012; Karagiannis et al., 2014)
- Reduced UTI’s as compared to the control group (Murray et al., 2016)
There are some really nice outcomes associated with these programs. Frazier has been documenting their outcomes on their website for years. They consistently document increased hydration with less dehydration, increased patient satisfaction, and no increase in pneumonia rates with the introduction of the protocol.
- All but one study reported no increase in pneumonia rates
- Karagiannis et al., 2011) reported a 14.3% pneumonia rate in protocol users with risk attributed to patients with degenerative conditions and reduced mobility/bedbound
Since Frazier started publishing its results, we have also seen some peer-reviewed research. The research is clear in terms of increased fluid intake equals an increased quality of life. The one study that documented an increase in pneumonia rates reported that increase was for inpatients with degenerative conditions who had significant reductions in mobility. That certainly would be a risk factor.
Water Protocols-Possible Exclusion Criteria
- Impulsivity
- Significantly impaired cognition
- Severe coughing
- Active pneumonia, oral infection
- Poor oral hygiene despite interventions
- Reduced mobility
- Degenerative condition
- Lung disease
(Frey et al., 2011; Carlaw et al., 2012; Karagiannis et al., 2011; Karagiannis et al., 2014; Murray et al., 2016; Pooyania et al., 2015)
These are some other risk factors that we can think about. These exclusionary criteria come from the peer-reviewed research. One example is someone who is coughing all the time with a thin liquid and is not comfortable. Another exclusion would be someone who cannot get their oral hygiene done. People who have impaired cognition and cannot understand why they cannot get water all the time would be another. I would encourage you to look at this research. It is fairly compelling.
To view the complete article and earn CEUs, become a member.
